Request Demo
Last update 08 May 2025
SMS synthase x SGMS2
Last update 08 May 2025
Basic Info
Related Targets |
Related
1
Drugs associated with SMS synthase x SGMS2CN119320385
Patent MiningTarget |
Mechanism SGMS2 inhibitors |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhaseDiscovery |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with SMS synthase x SGMS2
Login to view more data
100 Translational Medicine associated with SMS synthase x SGMS2
Login to view more data
0 Patents (Medical) associated with SMS synthase x SGMS2
Login to view more data
188
Literatures (Medical) associated with SMS synthase x SGMS201 Mar 2025·The FEBS Journal
Hypoxia‐induced increase in sphingomyelin synthase 2 aggravates ischemic skeletal muscle inflammation
Article
Author: Yasui, Hironobu ; Murakami, Hironobu ; Fukuyama, Tomoki ; Yamashita, Tadashi ; Naya, Yuko ; Aihara, Naoyuki ; Kamiie, Junichi ; Mizugaki, Hinano ; Nagane, Masaki ; Sato‐Akaba, Hideo ; Inanami, Osamu ; Kuppusamy, Periannan ; Kmiec, Maciej ; Yasuda, Ibuki ; Mizunoya, Wataru
01 Mar 2025·Bone Reports
A novel SGMS2 mutation associated with high bone mass; description of an affected family with recurrent fragility fractures
Article
Author: Prajapti, Ashka ; Pande, Minal ; Vyas, Parin ; Katam, Kishore K ; Kotecha, Udhaya ; Kedar, Ketki ; Patra, Shinjan ; Jena, Sweekruti
01 Mar 2025·Gastroenterology
Stromal Stiffness-Regulated IGF2BP2 in Pancreatic Cancer Drives Immune Evasion via Sphingomyelin Metabolism
Article
Author: Zhou, Cong ; Zhang, Zifeng ; Chen, Chen ; Tan, Zhen ; Rong, Zeyin ; He, Qing ; Liu, Xiaomeng ; Wang, Wei ; Liu, Yuan ; Liao, Yingna ; Chen, Yueyue ; Li, Yangyi ; Shi, Si ; Xu, Jin ; Lei, Yubin ; Lu, Siyuan ; Tang, Rong ; Yu, Xianjun ; Du, Qiong ; Zhang, Chaoyi ; Wu, Zijian ; Xiao, Mingming ; Li, Pengcheng
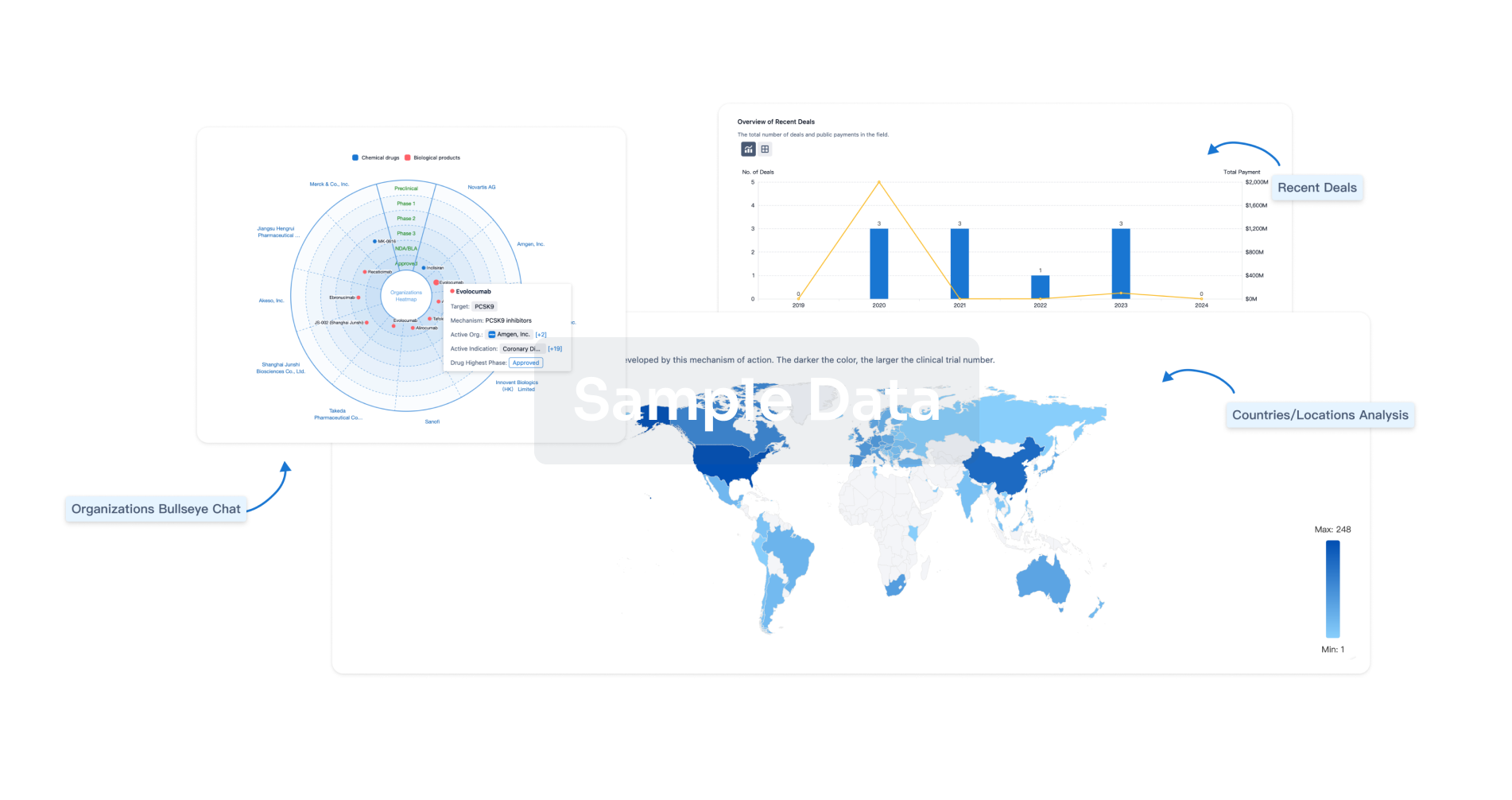
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
