Request Demo
Last update 08 May 2025
Nav1.9 x Nav1.8 x Nav1.7
Last update 08 May 2025
Related
1
Drugs associated with Nav1.9 x Nav1.8 x Nav1.7Target |
Mechanism Nav1.7 blockers [+2] |
Active Org.- |
Originator Org. |
Active Indication- |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
4
Clinical Trials associated with Nav1.9 x Nav1.8 x Nav1.7JPRN-jRCT2061200046
An exploratory Phase I/II study of ANP-230 to evaluate the safety, efficacy and pharmacokinetics in patients with infantile episodic limb pain
Start Date18 Jan 2021 |
Sponsor / Collaborator- |
ISRCTN02543559
A phase 1 study to investigate the effect of single and repeated doses of DSP-2230/placebo on renal function in healthy subjects
Start Date03 Oct 2013 |
Sponsor / Collaborator |
ISRCTN80154838
A randomised, double-blind, placebo-controlled, four-way crossover, two-part study investigating the pharmacodynamic effect of DSP-2230 using the ID Capsaicin and UVB models in healthy male subjects, using pregabalin and ibuprofen lysine as positive controls.
Start Date07 Jan 2013 |
Sponsor / Collaborator |
100 Clinical Results associated with Nav1.9 x Nav1.8 x Nav1.7
Login to view more data
100 Translational Medicine associated with Nav1.9 x Nav1.8 x Nav1.7
Login to view more data
0 Patents (Medical) associated with Nav1.9 x Nav1.8 x Nav1.7
Login to view more data
101
Literatures (Medical) associated with Nav1.9 x Nav1.8 x Nav1.703 Mar 2025·Journal of General Physiology
Nociceptor sodium channels shape subthreshold phase, upstroke, and shoulder of action potentials
Article
Author: Maxion, Anna ; Köster, Phil Alexander ; Stiehl, Thomas ; Namer, Barbara ; Leipold, Enrico ; Tigerholm, Jenny ; Lampert, Angelika
01 Mar 2025·Molecular Pain
Exploring novel non-opioid pathways and therapeutics for pain modulation
Review
Author: J, Sliter ; Alessi, Isabella ; CH, Palacio ; RJ, Ryznar ; Banton, Kaysie L ; C, Zaw-mon ; D, Bar-Or
01 Mar 2025·Molecular Pain
In silico
exploration of bioactive secondary metabolites with anesthetic effects on sodium channels Nav 1.7, 1.8, and 1.9 in painful human dental pulp
Article
Author: Kuruniyan, Mohamed Saheer ; Saini, Ravinder S ; Heboyan, Artak ; Binduhayyim, Rayan Ibrahim H
3
News (Medical) associated with Nav1.9 x Nav1.8 x Nav1.701 Feb 2024
Pictured: Rows of white pill bottles on a white surface/iStock, Androlia
With the opioid epidemic continuing to ravage the U.S., Vertex's announcement Tuesday that its non-opioid pain treatment VX-548 led to “significant improvement” in pain in two Phase III trials was widely hailed as a breakthrough. But the investigational drug did miss the first key secondary endpoint: superiority to a combination of the opioid hydrocodone bitartrate and Tylenol—a duo branded as Vicodin. This raises the question: Is it possible to do better?
Both trials—one testing VX-548 following abdominoplasty (tummy tuck) surgery, the other following bunionectomy surgery—hit the primary endpoint of statistically significant reduction of pain intensity from 0 to 48 hours. VX-548 failed, however, to beat Vicodin on the same scale.
During an investor call Tuesday, analysts also questioned the drug’s performance on another key secondary endpoint: median time to pain relief. In both indications, VX-548 had a “more rapid onset to meaningful pain relief” than placebo, Vertex reported, with median time to pain relief being two hours in tummy tuck patients and four hours in bunionectomy patients versus eight hours for the placebo group. Analysts on the call also appeared to be seeking faster time to pain relief, with Leerink Partners’ David Risinger asking if Vertex’s Phase I NaV1.8 inhibitors may offer a quicker onset.
Vertex CEO Reshma Kewalramani responded, saying, “If it is possible to get even better than VX-548, we are determined to be the ones who do so.”
Stuart Arbuckle, the company’s chief operating officer, also responded to questions from analysts, including how payors would respond to the drug’s efficacy. The “significant adverse events” and addictive potential associated with opioids are a major deterrent, he noted, adding that he believes payors will “warmly welcome the advent of a truly non-opioid pain med as this compelling combination of efficacy and safety and tolerability.”
When pressed for further details on the missed endpoint, Vertex representatives directed BioSpace to the investor call.
The Second Generation
VX-548 is a novel NaV1.8 pain signal inhibitor with a rich history. “The mechanistic evidence for [NaV1.8], even in the year 2001, was crystal clear,” said Stephen Waxman, a professor of neurology at Yale School of Medicine. “If you could shut it off, you had a good chance of attenuating pain.” This is around the time Vertex began its efforts against NaV1.8, which would ultimately yield VX-548, Waxman said.
Waxman, whose work contributed to the revelation that the NaV1.7, NaV1.8 and NaV1.9 sodium channels played a central role in pain signaling, highlighted three possible reasons for VX-548’s failure to beat Vicodin.
“One possibility is that [Vertex] did a good job on dosing but didn’t get it precisely right,” he said. “There could have been a higher dose with higher efficacy.” A second possibility, he said, is that a second-generation drug “will have more potency, more effective distribution, fewer side effects, be able to be dosed better and give better efficacy.”
Lastly, Waxman suggested that NaV1.8 may be “important enough in pain signaling that you get this degree of reduction of pain when it is blocked, but there is some redundancy in the pain pathway, so block of NaV1.8 reduces pain but does not totally abolish it.”
He likened VX-548 to the early days of the statin drugs. “The very first statin drugs worked, but in retrospect, they were not optimal, and the real bang for the buck in terms of societal impact was in the second and third-generation drugs,” he said. “And that’s where I think we are right now.”
As for what a second-generation drug might look like, Waxman noted that there are many approaches to targeting NaV1.8, including small-molecule blockers, peptide blockers, toxin derivatives, antibodies, knockdown therapies and gene therapy approaches.
“Now that we know that [NaV1.8] is a druggable target and we know that blocking it reduces pain, we have proof of concept in humans,” Waxman said. “That raises the exciting question of whether there are there other ways to attack 1.8, and there undoubtedly are. It is a very exciting time in the search for new, non-addictive pain medications.”
Heather McKenzie is a senior editor at BioSpace. You can reach her at heather.mckenzie@biospace.com. Also follow her on LinkedIn.
Phase 3Clinical ResultPhase 1
15 Nov 2022
Opioids reduce the symptoms of pain, not the underlying mechanism. Moreover, these drugs damage the reward pathway in the brain and can lead to addiction. Fortunately, opioids are not the only pharmaceutical option for treating pain: Non-addictive painkillers are widely available over the counter and by prescription. But research suggests that prescription painkillers, whether opioid-based or not, only work sufficiently in about 70% of patients. We need better options.
Humans’ relationship with opioids is ancient. It began 8,000 years ago when humans started using opioids as medicine in a less potent but still abusable form. The problems with opioid use crescendoed in recent decades, as broader indications for, and higher doses of, these drugs led to today’s epidemic, which has impacted countless lives.
Spurred by the opioid epidemic, scientists today are diving deeper into the neurobiological mechanisms of pain. They aim to find new druggable targets for treating pain effectively without causing addiction. This new generation of drugs could sidestep the dopamine and opioid pathways entirely by directly targeting the nociceptor pathway—a network of neurons all over the body responsible for mediating pain signaling. By carefully examining these drug candidates in humans, animals, and in vitro model systems, researchers hope to develop a more targeted class of painkillers that can help reduce reliance on addictive substances.
The link between pain and addiction
On the physiological level, chronic pain and addiction result from complementary neural feedback loops fueled by the opioid and dopamine systems. First, chronic pain may develop after repeated stress, inflammation, or acute injury, while addiction results from repeated exposure to an addictive substance. Both trigger epigenetic alterations in gene expression and protein localization within neurons. But, while chronic pain mainly involves changes within pain-sensing circuits, addiction causes additional changes in the reward center of the brain. Opioids operate by dulling pain perception in the brain, but they also act unnecessarily on the reward pathway, which is what makes them addictive. Therefore, painkillers that affect pain signaling at the site of pain and do not impact the reward pathway would offer a therapeutic benefit without causing additional harm.
Techniques used to study chronic pain
Scientists have used a variety of approaches to examine the effects of new pain-killing drug candidates on nociceptor signaling. Standard methods include structural modeling of receptors and ligands, behavioral evaluation, functional magnetic resonance imaging (fMRI), and electrophysiology. Together, these methods assess if a drug has the appropriate effect on brain activity and reduces pain.
Electrophysiology plays a critical role in the screening of therapeutic candidates. This technique enables researchers to examine how compounds impact the electrical activity of neurons and neural circuits. For these experiments, researchers grow dorsal root ganglion neurons and use inflammation-inducing compounds to cause the neurons to fire as if they were signaling inflammatory pain. Researchers subsequently treat the neurons with pain-killing drug candidates and monitor them for a reduction in neuronal activity.
However, conventional electrophysiological methods, such as patch-clamp, are low throughput, making it challenging to discover and test novel drug candidates efficiently. For this labor-intensive method, a highly trained scientist uses a micropipette to manipulate an individual cell and measure its electrochemical activity. Data collection is also limited as researchers can only examine each neuron for about an hour before the cell dies. Similarly, fMRI and behavioral studies return other types of high-quality data, but also at a slow pace. More recently, however, scientists are accelerating therapeutic discovery with a new kind of analysis using bioelectronic assays.
In bioelectronic assays, live neurons grow in a multiwell plate containing multielectrode arrays (MEAs) at the bottom of each well that continuously record the cells’ activity. Instead of measuring a single cell, these non-invasive bioelectronic assays can measure activity over time throughout a neuronal network. Researchers may conduct bioelectronic assays on generic cell lines or cell lines derived from a specific patient. Bioelectronic analysis of patient-specific models of chronic pain has helped accelerate the discovery of new painkillers.
A targeted search to find new painkillers
To develop a non-addictive painkiller, scientists have been searching for proteins that appear on pain neurons but not in the reward pathway, and this has been no small task. However, researchers have identified specific genes that fit the bill by studying rare, pain-related genetic disorders.
The sodium channels, Nav1.7, Nav1.8, and Nav1.9, have critical roles in pain-sensing, and early work uncovered the genes coding for these proteins. (Akopian, Roza, Yang, Cummins, Fjell, Wood). These channels make optimal pain-killing targets because they reside only in the dorsal root ganglion. Ideally, compounds that target these channels will dull pain without causing dependence. In a landmark study, scientists characterized the painful condition known as “burning man syndrome” or Inherited Erythromelalgia (IEM), which is caused by a mutation in the gene for Nav1.7. This study was one of the first human studies confirming that gain-of-function mutations in these genes cause disorders associated with heightened pain. Conversely, researchers found that loss-of-function mutations render an individual less able to sense pain.16 Armed with this knowledge, researchers could finally conduct targeted studies to search for a novel class of painkillers.
An early pharmacological breakthrough came out of the Waxman lab in 2012.17,18 The Waxman team was studying two patients with IEM, and structural modeling of the mutated S241T Nav1.7 channel predicted that these individuals would be responsive to the anti-epileptic drug carbamazepine. fMRI assessments revealed that carbamazepine treatment reduced brain activity associated with pain signaling in both patients. Furthermore, both patients reported significant pain reduction: For one patient, carbamazepine treatment cut the amount of time they spent in pain per day in half, with fewer instances of waking up in pain at night. The other patient reported that the drug reduced time in pain by about 85 percent. A bioelectronic analysis confirmed this positive effect at the cellular level: the Waxman group cultured dorsal root ganglion neurons expressing the same Nav1.7 sodium channel mutation of the patients and exposed them to heat, a stimulus that causes pain in individuals with IEM. Heat exposure increased neuronal firing, and carbamazepine treatment reduced the heat-induced activity, mirroring its clinical effects.
Since then, researchers have advanced a dozen new compounds that selectively block the Nav1.7 and Nav1.8 sodium channels and one that blocks Nav1.9 to clinical trials, with three in phase 3. These researchers aim to identify treatments for conditions ranging from IEM to diabetic neuropathy. Overall, these compounds do not appear to be addictive and do not produce dangerous side effects; however, they show varying efficacy in reducing pain. Therefore, the search continues to uncover potential new Nav1.7 and Nav1.8 inhibitors like small molecules and therapeutic antibodies. Some researchers have designed high-throughput screens based on bioelectronic assays to take on the search. While these screening systems are still in their infancy, once up and running, they promise to greatly accelerate the identification of promising, physiologically relevant painkiller candidates.
Conclusion
The body of research seeking a better class of pain relievers is relatively young, but it’s rapidly advancing. Regardless of which method uncovers new painkiller targets, researchers must assess these novel compounds for addictive properties and unexpected side effects. These efforts will yield painkillers that operate through a more effective, targeted mechanism. As time goes on, individuals may have access to a more diverse selection of non-addictive painkillers, and physicians will be able to assign patients a treatment based on their unique physiological makeup. Overall, this promising field of research stands to improve how we treat pain and reduce the number of individuals who rely on opioids. With scientists seeking to divorce pain from addiction, the future of pain treatment is increasingly bright.
Phase 3Clinical Result
02 Jun 2022
SURESNES, France--(BUSINESS WIRE)-- European biotech AlgoTx, an innovator in complex pain therapy, today announces the U.S. Food and Drug Administration (FDA) cleared its Investigational New Drug Application (IND) for Phase 2 candidate ATX01 in the treatment of Chemotherapy-Induced Peripheral Neuropathy (CIPN).
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20220601005198/en/
Over half of cancer patients treated with chemotherapy develop CIPN and experience sensory symptoms and pain in the feet and hands including loss of sensitivity, tingling, cold allodynia, intense burning and shooting pain that can persist for months to years after treatment. CIPN is a leading cause of modification or interruption of chemotherapy. To this date, no therapeutic approach has offered a satisfactory response for patients and their caregivers, oncologists, neurologists and pain specialists.
ATX01 enjoys solid intellectual property including its patented topical formulation of amitriptyline designed to inhibit pain messaging by directly targeting small sensory nerve fibers in the skin which generate and conduct pain messages from the peripheral nervous system to the spine and brain. Indeed ATX01’s breakthrough pre-clinical investigation evidenced the anti-nociceptive activity of amitriptyline on voltage-gated sodium-channels Nav1.7, Nav1.8 and Nav1.9 and on peripheral sensory nerve fibers A∂ and C. ATX01’s Phase 1 program established safety in healthy volunteers and limited systemic passage designed to avoid the systemic side-effects of oral and injectable compounds.
Philippe Picaut, Chief Development Officer, commented: “This IND is a validation of our development work to date, and we are now eager to work alongside a large team of enthusiastic investigators in the US and Europe who share our goal of bringing relief to CIPN patients.”
FDA’s IND clearance opens the way for the planned Phase 2 study, a multi-center, double-blind, randomized, placebo-controlled study of ATX01 in the pain of CIPN in adult cancer survivors. The study aims to establish ATX01’s efficacy and safety in CIPN patients and will be conducted in the US and Europe.
“This IND is a major milestone for CIPN patients and for AlgoTx. In an indication without therapeutic solutions, ATX01’s highly differentiated mode of action has the potential to finally bring relief to patients with CIPN,” says Stéphane Thiroloix, AlgoTx’s founder and CEO.
About AlgoTx : AlgoTx is a European biotech founded in 2018 to develop innovative solutions for complex pain, whose Series A funding was led by Bpifrance and Omnes Capital. ATX01 is entering Phase 2 in painful peripheral neuropathy.
www.algotx.com
Clinical Trial ApplicationDrug Review
Analysis
Perform a panoramic analysis of this field.
login
or
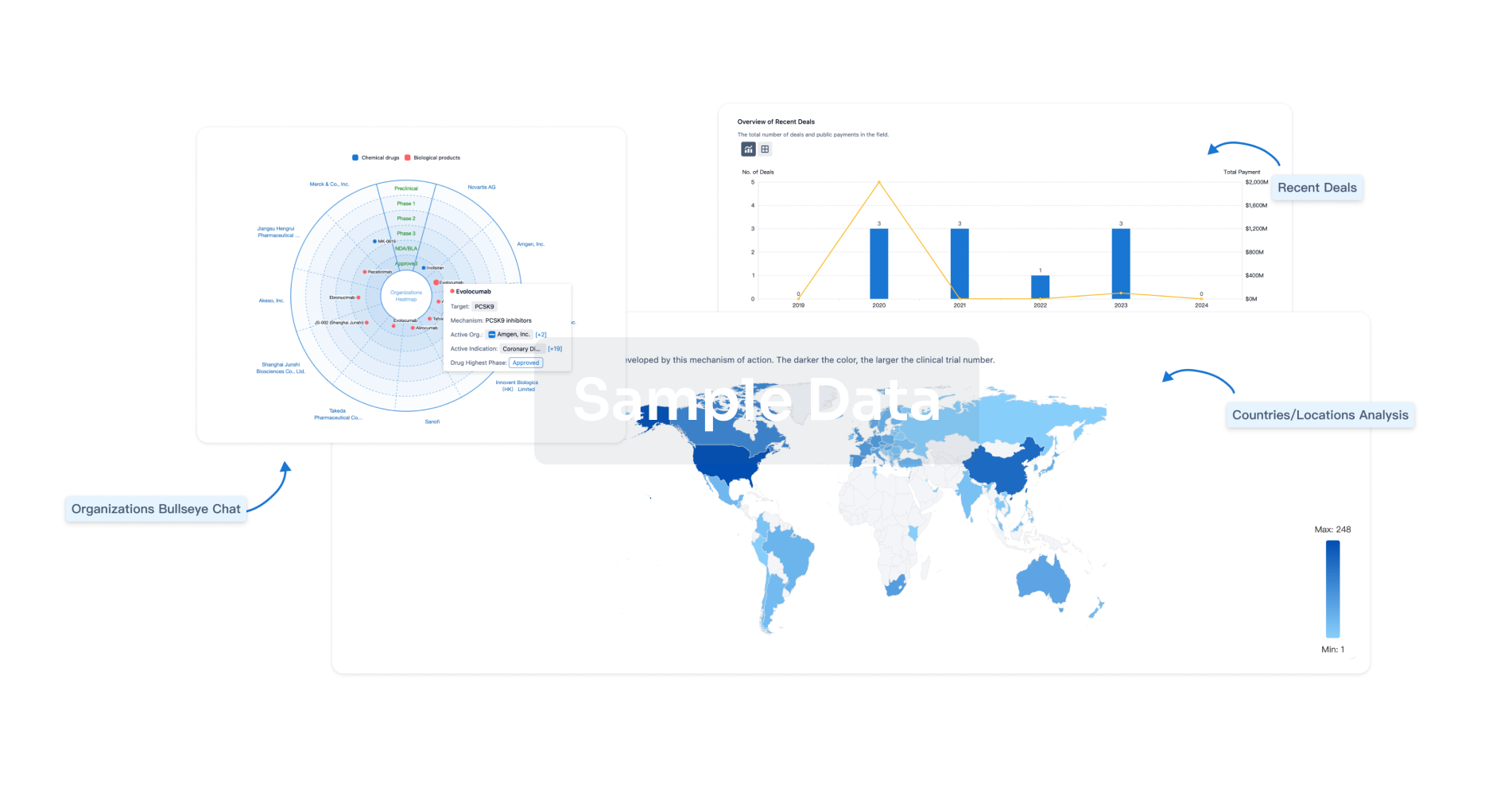
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
