Request Demo
Last update 08 May 2025
PXR
Last update 08 May 2025
Basic Info
Synonyms BXR, NR1I2, Nuclear receptor subfamily 1 group I member 2 + [10] |
Introduction Nuclear receptor that binds and is activated by variety of endogenous and xenobiotic compounds. Transcription factor that activates the transcription of multiple genes involved in the metabolism and secretion of potentially harmful xenobiotics, drugs and endogenous compounds. Activated by the antibiotic rifampicin and various plant metabolites, such as hyperforin, guggulipid, colupulone, and isoflavones. Response to specific ligands is species-specific. Activated by naturally occurring steroids, such as pregnenolone and progesterone. Binds to a response element in the promoters of the CYP3A4 and ABCB1/MDR1 genes. |
Related
14
Drugs associated with PXRTarget |
Mechanism PXR agonists |
Active Org.- |
Originator Org.- |
Active Indication- |
Inactive Indication- |
Drug Highest PhaseApproved |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism ELA2 inhibitors [+1] |
Active Org.- |
Originator Org.- |
Active Indication |
Inactive Indication- |
Drug Highest PhaseApproved |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Mechanism 11β-HSD1 inhibitors [+2] |
Active Org.- |
Originator Org.- |
Active Indication |
Inactive Indication- |
Drug Highest PhaseApproved |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
399
Clinical Trials associated with PXRNCT06634056
Pneumonitis Prevention Protocol Using Pentoxifylline and α-tocopherol in Stage III Non-Small Cell Lung Cancer Patients Undergoing Chemoradiation
Currently, the standard of care treatment for newly diagnosed, inoperable stage III non-small cell lung cancer is radiotherapy (RT) with concurrent chemotherapy, followed by immune checkpoint inhibitors (ICI). RT is a highly effect local treatment. However, high doses of radiation used in curative settings can cause adverse side effects. The most common RT side effect in lung cancer is Radiation Induced Lung Injury (RILI), which can manifest as pneumonitis and/or pulmonary fibrosis. Lung injury can negatively impact patients' well-being and quality of life, and may lead to increased mortality. Risk of lung injury is particularly increased when patients are treated with a combination of treatments (i.e., RT, chemotherapy, and ICI). The drug Pentoxifylline (in combination with α-Tocopherol (Vitamin E)) has been shown to prevent/alter the progression of lung injury and there is a growing body of evidence to support the safety and efficacy of phosphodiesterase inhibitors in cancer treatment. The proposed study aims to determine if the addition of Pentoxifylline, given in combination with α-Tocopherol (Vitamin E), to standard of care treatment will reduce side effects related to lung injury and improve quality of life in this study population.
Start Date30 May 2025 |
Sponsor / Collaborator |
CTRI/2025/04/084228
A randomized, controlled, parallel-arm, open-label clinical trial to evaluate the safety and efficacy of Hair Serum alone or in combination with Hair vitamin gummies in reducing hair fall and improving hair growth in adult male and female participants. - NIL
Start Date16 Apr 2025 |
Sponsor / Collaborator |
NCT06871904
Exploring the Fibrosis-Modulating Potential of Metformin and Pirfenidone in Oral Submucous Fibrosis: Molecular Mechanisms to Clinical Applications
The goal of this clinical trial is to learn if metformin and antifibrotic drugs (pirfenidone) can modulate fibrosis and improve treatment outcomes in patients with oral submucous fibrosis (OSF). The study also aims to investigate the molecular mechanisms underlying their effects on exosome secretion and protein expression.
The main questions it aims to answer are:
Do metformin and antifibrotic drugs alter exosome secretion and biological activity in OSF cell lines? What molecular pathways are influenced by these drugs in modulating fibrosis? Does treatment with metformin and antifibrotic drugs improve clinical outcomes in OSF patients? Researchers will compare metformin and antifibrotic drug treatment groups to a control group to see if these drugs lead to significant changes in fibrosis-related exosomal protein expression and clinical improvement in OSF patients.
Participants will :
Undergo in vitro experiments on OSF cell lines to analyze drug effects using qPCR, Western Blot, and LCMS for protein profiling.
Participate in a randomized, double-blind clinical trial where they receive metformin, antifibrotic drugs, or a placebo.
Undergo clinical evaluations and laboratory tests to assess treatment efficacy. This study aims to develop an affordable and effective fibrosis-targeted therapy for OSF by repurposing metformin, potentially improving patient outcomes and reducing the risk of malignant transformation.
The main questions it aims to answer are:
Do metformin and antifibrotic drugs alter exosome secretion and biological activity in OSF cell lines? What molecular pathways are influenced by these drugs in modulating fibrosis? Does treatment with metformin and antifibrotic drugs improve clinical outcomes in OSF patients? Researchers will compare metformin and antifibrotic drug treatment groups to a control group to see if these drugs lead to significant changes in fibrosis-related exosomal protein expression and clinical improvement in OSF patients.
Participants will :
Undergo in vitro experiments on OSF cell lines to analyze drug effects using qPCR, Western Blot, and LCMS for protein profiling.
Participate in a randomized, double-blind clinical trial where they receive metformin, antifibrotic drugs, or a placebo.
Undergo clinical evaluations and laboratory tests to assess treatment efficacy. This study aims to develop an affordable and effective fibrosis-targeted therapy for OSF by repurposing metformin, potentially improving patient outcomes and reducing the risk of malignant transformation.
Start Date01 Apr 2025 |
Sponsor / Collaborator  Ziauddin University Ziauddin University [+1] |
100 Clinical Results associated with PXR
Login to view more data
100 Translational Medicine associated with PXR
Login to view more data
0 Patents (Medical) associated with PXR
Login to view more data
3,565
Literatures (Medical) associated with PXR01 Aug 2025·Phytochemistry
SMART-assisted discovery of butenolides from the marine-derived Aspergillus sp. NBU4698 with multidrug resistance reversing and anti-inflammatory activity
Article
Author: Zhao, Hang ; Zhou, Ziyi ; Yuan, Wei ; Ding, Lijian ; Feng, Fangjian ; Chen, Lixin ; Lin, Wenhan ; Zhou, Zhiyan ; He, Shan ; Ju, Zhiran ; Naman, C Benjamin
01 Jul 2025·Critical Reviews in Oncology/Hematology
Pharmacogenomics in pediatric oncology patients with solid tumors related to chemotherapy-induced toxicity: A systematic review
Review
Author: Uvdal, Hanna ; Hansson, Paula ; Blacker, Christopher ; Wadelius, Mia ; Green, Henrik ; Ljungman, Gustaf
01 Jun 2025·Environmental Toxicology and Pharmacology
Comparison of the impact of chlordecone and its metabolite chlordecol on genes involved in pesticide metabolism in HepG2 cell line
Article
Author: Joubert, Olivier ; Djansugurova, Leyla ; El Sheikh Saad, Hanan ; Paul, Arnaud ; Cakir-Kiefer, Céline ; Huguet, Marion ; Fournier, Agnès ; Baratzhanova, Gulminyam
4
News (Medical) associated with PXR02 Jan 2024
Adds Clinical-Stage Product Pipeline, Expands Intranasal Drug Delivery Technologies,
Names Michael Redmond as President of Oragenics
TAMPA, Fla.--(BUSINESS WIRE)--Oragenics, Inc. (NYSE American: OGEN) (“Oragenics” or the “Company”) announces it has completed its previously announced acquisition of assets related to Odyssey Health, Inc.’s (OTCQB: ODYY) (“Odyssey”) proprietary neurological drug therapies and technologies.
The acquired assets include ONP-002 and a unique nasal delivery device, Odyssey’s lead concussion asset, believed to be a first-in-class intranasal drug under development for the treatment of moderate-to-severe concussion in the acute through subacute phases. In preclinical animal studies, the asset demonstrated rapid and broad biodistribution throughout the brain while simultaneously reducing swelling, inflammation and oxidative stress, along with an excellent safety profile. Results from animals treated with the drug post-concussion showed positive behavioral outcomes using various testing platforms including improved memory and sensory-motor performance, and reduced anxiety. ONP-002 has completed a Phase 1 clinical trial in healthy human subjects showing it is safe and well tolerated. Oragenics anticipates preparing for Phase 2 clinical trials to further evaluate ONP-002’s safety and efficacy.
Also included in the acquired assets are all of Odyssey’s rights and interest in ONP-001, believed to be a first-in-class neurosteroid being developed for the treatment of Niemann Pick Type-C Disease (NPC), as well as Odyssey’s proprietary powder formulation and its intranasal delivery device. Odyssey will retain its other assets and operations.
“We are delighted to complete this pivotal transaction following a favorable vote of shareholders at both companies. We expect that Odyssey’s neurological pipeline will significantly expand our market opportunity and believe its technology complements our expertise in intranasal drug delivery. This acquisition also addresses a significant and growing health concern. There are an estimated 5 million concussions annually in the U.S., with up to half going unreported, underscoring a substantial market opportunity for an efficacious treatment,” said Kim Murphy, Chief Executive Officer of Oragenics.
“Our decision to invest in this innovative therapy is driven by our commitment to pioneering solutions that build upon our expertise in intranasal drug delivery and our dedication to improving patient outcomes. These new pipeline candidates hold potential to deliver innovative treatments for millions affected by mTBI and NPC, and introduce Oragenics into a market that is projected to grow to $8.9 billion annually by 2027,” added Ms. Murphy.
In conjunction with the transaction, Michael Redmond, who has served as President and CEO of Odyssey since 2018, was named President of Oragenics. Mr. Redmond has 35 years of commercial experience with medical device companies, having held various sales and marketing leadership positions that helped accelerate growth at companies to multiples of their previous revenue and valuation. Mr. Redmond also has significant experience in raising capital and securing licensing and distribution deals with major biotech and pharmaceutical companies. In his new position, Mr. Redmond will oversee the growth of Oragenics’ neurology product pipeline and intranasal drug delivery technologies.
Additionally, the Odyssey management and development team that led the ONP-002 clinical trial design and implementation for the treatment of concussion, will continue to oversee research and development of the newly acquired neurology assets at Oragenics. The team has experience in conducting clinical trials, developing drug formulations and commercializing pharmaceutical products across a broad range of indications.
“I’m proud to join the executive team at Oragenics and look forward to continuing the development of ONP-002 and ultimately utilizing my experience in commercializing therapeutics. We intend to leverage our joint expertise and resources to expedite the development of this drug, with the goal of filling a critical gap in concussion care as we prepare for a Phase 2 clinical study in the first half of 2024. We believe this transaction also strengthens Oragenics’ research and development capabilities, including the integration of key members of Odyssey’s research and development team with the Oragenics team,” said Mr. Redmond.
About ONP-002
ONP-002 is a fully synthetic neurosteroid being developed to treat mTBI. In preclinical studies, the drug demonstrated equivalent or better neuroprotective effects compared with related neurosteroids. Animal models of concussion showed the drug reduces the behavioral pathology associated with brain injury symptoms such as memory impairment, anxiety and motor/sensory performance. Additionally, ONP-002 is lipophilic and can cross the blood-brain barrier to rapidly eliminate swelling, oxidative stress and inflammation while restoring proper blood flow.
About Mild Traumatic Brain Injury (mTBI)
Concussions are an unmet medical need that affects millions worldwide. Repetitive concussions can increase the risk of developing chronic traumatic encephalopathy and other neuropsychiatric disorders. It is estimated that 5 million concussions occur in the U.S. annually and that up to 50% go unreported. The worldwide incidence is estimated at 69 million per year. The global market for concussion treatment was valued at $6.9 billion in 2020 and is forecast to reach $8.9 billion by 2027, according to Grandview Research. Common settings for concussion include contact sports, military training and operations, motor vehicle accidents, children at play and elderly assistive-living facilities due to falls.
About Niemann-Pick Type C Disease
Niemann-Pick Type C disease is a rare neurodegenerative genetic disorder characterized by the inability of cells to metabolize and properly transport cholesterol and other lipids, leading to the abnormal accumulation in various tissues including brain tissue. The market for NPC therapeutics is expected to grow from $128 million in 2022 to $188 million in 2031 across the U.S., Germany and UKi.
Forward-Looking Statements
This communication contains “forward-looking statements” within the meaning of the safe harbor provisions of the U.S. Private Securities Litigation Reform Act of 1995 including, without limitation, statements regarding the ability of the Company to timely and successfully achieve the anticipated benefits of acquiring the Odyssey assets and the Company’s future performance, business prospects, events and product development plans. These forward-looking statements are based on management’s beliefs and assumptions and information currently available. The words “believe,” “expect,” “anticipate,” “intend,” “estimate,” “project” and similar expressions that do not relate solely to historical matters identify forward-looking statements. Investors should be cautious in relying on forward-looking statements because they are subject to a variety of risks, uncertainties, and other factors that could cause actual results to differ materially from those expressed in any such forward-looking statements. These factors include, but are not limited to, the following: the Company’s ability to advance the development of its product candidates under the timelines and in accord with the milestones it projects; the Company’s ability to obtain funding, non-dilutive or otherwise, for the development of its product candidates, whether through its own cash on hand, or another alternative source; the regulatory application process, research and development stages, and future clinical data and analysis, decisions by regulatory authorities, such as the FDA and investigational review boards, whether favorable or unfavorable; the potential application of our research and development candidates; the Company’s ability to obtain, maintain and enforce necessary patent and other intellectual property protection; the nature of competition and development relating to concussion treatments, treatments for NPC and COVID-19 immunization and therapeutic treatments and demand for vaccines and antibiotics; the Company’s expectations as to the outcome of preclinical studies, nasal administration, transmission, manufacturing, storage and distribution; other potential adverse impacts due to the global COVID-19 pandemic, such as delays in regulatory review, interruptions to manufacturers and supply chains, adverse impacts on healthcare systems and disruption of the global economy; and general economic and market conditions and risks, as well as other uncertainties described in our filings with the U.S. Securities and Exchange Commission. All information set forth in this communication is as of the date hereof. You should consider these factors in evaluating the forward-looking statements included in this communication and not place undue reliance on such statements. We do not assume any obligation to publicly provide revisions or updates to any forward-looking statements, whether as a result of new information, future developments or otherwise, should circumstances change, except as otherwise required by law.
i Source: GlobalData
Phase 1Clinical ResultAcquisitionExecutive ChangePhase 2
03 Nov 2023
Pictured: Pills organized in a digital pattern/iStock, EvilWata
When Alex Zhavoronkov launched Insilico Medicine in 2014, the company’s main focus was on using artificial intelligence as an alternative to animal testing for pharmaceutical research and development. Using deep learning, an advanced form of machine learning, the company aimed to predict how drug compounds would affect cells and what the side effects might be.
Fast forward to 2023, and Insilico has evolved into an end-to-end AI-driven biotech company, deploying AI from lead and target discovery through clinical trials. Insilico’s Pharma.AI platform, backed by $2 trillion in machine-readable research data, contains over 40 generative algorithms. The firm uncovered the intracellular “Target X” for idiopathic pulmonary fibrosis (IPF) using AI analysis, and subsequently developed a novel small molecule inhibitor, INS018_055, which has shown potential in preclinical studies for improved fibrotic disease treatment with fewer side effects. In August, it became the first drug fully generated by AI to enter a Phase II trial.
Making up the Pharma.AI platform, Insilico’s PandaOmics for target discovery, Chemistry42 for drug design and InClinico for clinical trial prediction “work together in an end-to-end feedback loop,” Zhavoronkov explained.
“However, safety of the target is accounted for at two different stages,” said Alex Aliper, president of Insilico. First, PandaOmics uses relevant existing information to find the safest and most promising therapeutic targets, while Chemsitry42 enables multi-parametric optimization of the molecules.
The latter includes ADMET predictors, a machine learning (ML) software tool, to assess how the body processes the generated molecule, covering aspects like absorption, distribution, metabolism, elimination and toxicity, as well as enzyme inhibition like cytochrome P450, which is involved in drug side effects. “Chemistry42 also has around 500 medicinal chemistry filters that filter out compounds with structural motifs known to be toxic,” Aliper told BioSpace.
“Our initial studies have indicated that INS018_055 has the potential to address some of the limitations of current IPF therapies—including unpleasant side effects—and we are hopeful that the data from our current and future clinical trials will confirm this belief,” Zhavoronkov said.
Schrödinger’s Selectivity
New York- and Germany–based Schrödinger focuses on the safety of small-molecule drugs. Its platform blends AI/ML efficiency with physics-based accuracy, enabling its specialists to design and synthesize desired molecules, thus reducing time and costs.
“In some cases, the clinical candidate has been selected after synthesizing just 100 molecules instead of the thousands made using traditional design approaches,” said Robert Abel, the company’s chief computational scientist.
In order to minimize drug side effects, Schrödinger uses its platform to design molecules that bind potently and selectively to the intended protein target versus related proteins, explained Karen Akinsanya, president of R&D, therapeutics at Schrödinger. “This approach allows us to find molecules that might provide a therapeutic benefit without binding to hERG, CYPs, PXR and other well-known off-target proteins that are well known to cause side effects,” she told BioSpace.
The hERG gene is crucial for heart rhythm regulation; CYPs, or cytochromes, are liver enzymes that metabolize drugs, potentially causing interactions; PXR, a cellular protein, helps process drugs and foreign substances by influencing enzyme production. These factors are vital in drug development and medication safety, Akinsanya said. “Protein structures, including binding sites, are crucial for our computational platform, but starting a drug discovery project often lacks enough experimental data for naive AI approaches due to the vast chemical space, which exceeds available data,” she explained. “Schrödinger addresses this by using advanced physics-based calculations to efficiently generate the needed binding affinity datasets.”
Both Insilico and Schrödinger use AI to discover drugs that they claim would be safer than those hunted down using non-AI methods. Big pharma players also entered this space a few years ago, either directly or by partnering with tech companies or incubating smaller AI-based startups. AstraZeneca collaborated with BenevolentAI to discover new targets and predict potential drug side effects by analyzing scientific literature, clinical trial data and biomedical databases.
Novartis employs AI for intelligent molecular design to develop safe molecules for patients. By analyzing various data sources, including chemical properties and biological interactions, the company aims to identify compounds with lower risk pro Meanwhile, Merck KGaA has been busy inking AI deals aimed at making safer medicines. In 2018, Merck struck an alliance with Canadian company Cyclica that uses the latter’s cloud-based technology to uncover new drug targets and identify off-target adverse effects. Then, in February 2022, the company announced a partnership to leverage Quris’ BioAI safety prediction platform, which uses miniaturized human tissues on a chip, nano-sensing and machine learning to predict the safety of drug candidates in humans.
Confidence and Caution
AI’s potential in drug development is often recognized with respect to saving time and money. However, its increasing deployment in drug safety studies elicits both confidence and caution from industry and researchers, according to experts such as Andreas Bender, a chemoinformatics researcher at the University of Cambridge, U.K.
Bender, who has been working with AstraZeneca on computational drug safety studies, said there is often a “tech push and a science pull” about AI. Although data collection becomes easier, understanding the data’s signal is more critical, he told BioSpace. “We have quite a lot of data, but we don’t understand much of that pile, like how certain biological mechanisms relate to a phenotype,” he said. Using AI to identify potential side effects is “like [finding] a needle in a haystack.”
Drug safety lies not just in how the molecule has been designed but also in other factors. For example, Bender explained, the use of excipients—the inert or slightly active substances used in formulating a drug compound into a drug product—and other additives can affect a drug’s safety profile, as can patient biology and environmental stimuli.
“There are mechanistic side effects that you know where they come from and what to do about, but there are also idiosyncratic side effects that you don’t know where they come from, so you cannot predict such adverse reactions using AI,” he said. Hence, along with machine learning, his group’s research also integrates chemical biology and human physiology to predict drug toxicity.
There are multiple other challenges, Bender continued, such as how different countries define specific side effects. “How do we translate, then, the [computational predictions] into decision-making?” he asked. “That integration is often where the real problems come from, and that’s why you always need to integrate computers with experiments—[to] follow up on predictions.”
Still, he said, AI-based predictions of drug safety could improve the drug development process. “It is, rather, about making better decisions. I’m not saying nothing works, but also not that everything works; just . . . that finding meaningful signals in drug safety prediction is statistically more difficult and depends on several [kinds of] data, so promises must be cautious and realistic.”
Vijay Shankar Balakrishnan is a freelance journalist based in Ludwigshafen, Germany. Reach him at LinkedIn.
Phase 2
30 Oct 2023
Pills organized in a digital pattern/iStock, EvilW
Alexandre Watanabe (EvilWata Imagery)/Getty Images
More and more companies are turning to artificial intelligence for drug safety prediction, but as with any new application of AI, experts urge caution.
Pictured: Pills organized in a digital pattern/
iStock
, EvilWata
When Alex Zhavoronkov launched Insilico Medicine in 2014, the company’s main focus was on using artificial intelligence as an alternative to animal testing for pharmaceutical research and development. Using deep learning, an advanced form of machine learning, the company aimed to predict how drug compounds would affect cells and what the side effects might be.
Fast forward to 2023, and Insilico has evolved into an end-to-end AI-driven biotech company, deploying AI from lead and target discovery through clinical trials. Insilico’s Pharma.AI platform, backed by $2 trillion in machine-readable research data, contains over 40 generative algorithms. The firm uncovered the intracellular “
Target X
” for idiopathic pulmonary fibrosis (IPF) using AI analysis, and subsequently developed a novel small molecule inhibitor, INS018_055, which has shown potential in preclinical studies for improved fibrotic disease treatment with fewer side effects. In August, it became the first drug fully generated by AI to enter
a Phase II trial
.
Making up the Pharma.AI platform, Insilico’s PandaOmics for target discovery, Chemistry42 for drug design and InClinico for clinical trial prediction “work together in an end-to-end feedback loop,” Zhavoronkov explained.
“However, safety of the target is accounted for at two different stages,” said Alex Aliper, president of Insilico. First, PandaOmics uses relevant existing information to find the safest and most promising therapeutic targets, while Chemsitry42 enables multi-parametric optimization of the molecules.
The latter includes ADMET predictors, a machine learning (ML) software tool, to assess how the body processes the generated molecule, covering aspects like absorption, distribution, metabolism, elimination and toxicity, as well as enzyme inhibition like cytochrome P450, which is involved in drug side effects. “Chemistry42 also has around 500 medicinal chemistry filters that filter out compounds with structural motifs known to be toxic,” Aliper told
BioSpace
.
“Our initial studies have indicated that INS018_055 has the potential to address some of the limitations of current IPF therapies—including unpleasant side effects—and we are hopeful that the data from our current and future clinical trials will confirm this belief,” Zhavoronkov said.
Schrödinger’s Selectivity
New York- and Germany–based
Schrödinger
focuses on the safety of small-molecule drugs. Its platform blends AI/ML efficiency with physics-based accuracy, enabling its specialists to design and synthesize desired molecules, thus reducing time and costs.
“In some cases, the clinical candidate has been selected after synthesizing just 100 molecules instead of the thousands made using traditional design approaches,” said Robert Abel, the company’s chief computational scientist.
In order to minimize drug side effects, Schrödinger uses its platform to design molecules that bind potently and selectively to the intended protein target versus related proteins, explained Karen Akinsanya, president of R&D, therapeutics at Schrödinger. “This approach allows us to find molecules that might provide a therapeutic benefit without binding to hERG, CYPs, PXR and other well-known off-target proteins that are well known to cause side effects,” she told
BioSpace
.
The hERG gene is crucial for heart rhythm regulation; CYPs, or cytochromes, are liver enzymes that metabolize drugs, potentially causing interactions; PXR, a cellular protein, helps process drugs and foreign substances by influencing enzyme production. These factors are vital in drug development and medication safety, Akinsanya said. “Protein structures, including binding sites, are crucial for our computational platform, but starting a drug discovery project often lacks enough experimental data for naive AI approaches due to the vast chemical space, which exceeds available data,” she explained. “Schrödinger addresses this by using advanced physics-based calculations to efficiently generate the needed binding affinity datasets.”
Both Insilico and Schrödinger use AI to discover drugs that they claim would be safer than those hunted down using non-AI methods. Big pharma players also entered this space a few years ago, either directly or by partnering with tech companies or incubating smaller AI-based startups.
AstraZeneca collaborated with BenevolentAI
to discover new targets and predict potential drug side effects by analyzing scientific literature, clinical trial data and biomedical databases.
Novartis employs AI
for intelligent molecular design to develop safe molecules for patients. By analyzing various data sources, including chemical properties and biological interactions, the company aims to identify compounds with lower risk pro Meanwhile, Merck KGaA has been busy inking AI deals aimed at making safer medicines. In 2018, Merck struck an
alliance
with Canadian company Cyclica that uses the latter’s cloud-based technology to uncover new drug targets and identify off-target adverse effects. Then, in February 2022, the company announced a
partnership
to leverage Quris’ BioAI safety prediction platform, which uses miniaturized human tissues on a chip, nano-sensing and machine learning to predict the safety of drug candidates in humans.
Confidence and Caution
AI’s potential in drug development is often recognized with respect to saving time and money. However, its increasing deployment in drug safety studies elicits both confidence and caution from industry and researchers, according to experts such as Andreas Bender, a chemoinformatics researcher at the University of Cambridge, U.K.
Bender, who has been working with AstraZeneca on computational drug safety studies, said there is often a “tech push and a science pull” about AI. Although data collection becomes easier, understanding the data’s signal is more critical, he told
BioSpace
. “We have quite a lot of data, but we don’t understand much of that pile, like how certain biological mechanisms relate to a phenotype,” he said. Using AI to identify potential side effects is “like [finding] a needle in a haystack.”
Drug safety lies not just in how the molecule has been designed but also in other factors. For example, Bender explained, the use of excipients—the inert or slightly active substances used in formulating a drug compound into a drug product—and other additives can affect a drug’s safety profile, as can patient biology and environmental stimuli.
“There are mechanistic side effects that you know where they come from and what to do about, but there are also idiosyncratic side effects that you don’t know where they come from, so you cannot predict such adverse reactions using AI,” he said. Hence, along with
machine learning
, his group’s research also integrates chemical biology and human physiology to predict
drug toxicity
.
There are multiple other challenges, Bender continued, such as how different countries define specific side effects. “How do we translate, then, the [computational predictions] into decision-making?” he asked. “That integration is often where the real problems come from, and that’s why you always need to integrate computers with experiments—[to] follow up on predictions.”
Still, he said, AI-based predictions of drug safety could improve the drug development process. “It is, rather, about making better decisions. I’m not saying nothing works, but also not that everything works; just . . . that finding meaningful signals in drug safety prediction is statistically more difficult and depends on several [kinds of] data, so promises must be cautious and realistic.”
Vijay Shankar Balakrishnan is a freelance journalist based in Ludwigshafen, Germany. Reach him at
LinkedIn
.
Phase 2
Analysis
Perform a panoramic analysis of this field.
login
or
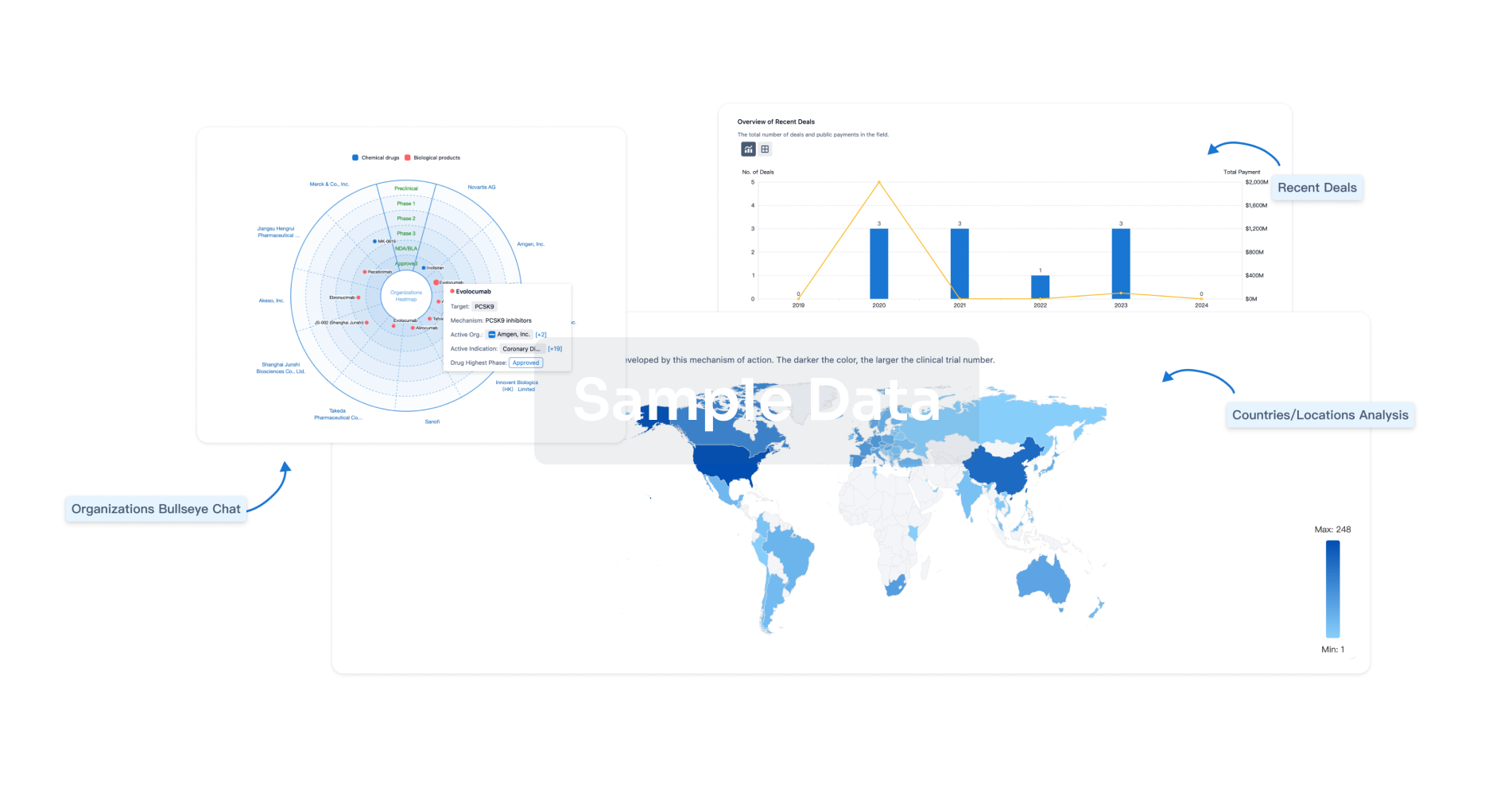
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free