Request Demo
Last update 08 May 2025
IDH1 x NAMPT
Last update 08 May 2025
Related
1
Drugs associated with IDH1 x NAMPTTarget |
Mechanism IDH1 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with IDH1 x NAMPT
Login to view more data
100 Translational Medicine associated with IDH1 x NAMPT
Login to view more data
0 Patents (Medical) associated with IDH1 x NAMPT
Login to view more data
7
Literatures (Medical) associated with IDH1 x NAMPT13 Jun 2024·Journal of Medicinal Chemistry
Discovery of Novel Dual Inhibitors Targeting Mutant IDH1 and NAMPT for the Treatment of Glioma with IDH1Mutation
Article
Author: Ma, Tianfang ; Li, Chunzheng ; Gui, Gang ; Qin, Anqi ; Wang, Xiaoyu ; Wen, Fei ; Zha, Xiaoming ; Chen, Hui
01 Jan 2021·Free Radical Biology and MedicineQ2 · MEDICINE
NAD+ depletion radiosensitizes 2-DG-treated glioma cells by abolishing metabolic adaptation
Q2 · MEDICINE
Article
Author: Yu, Jiahua ; Zhang, Haowen ; Wang, Zhongmin ; Wang, Chen ; Zhang, Wei ; Yin, Narui ; Shi, Xiaolin ; Gu, Cheng ; Liu, Fenju ; Ren, Huangge
04 Sep 2018·Proceedings of the National Academy of SciencesQ1 · CROSS-FIELD
Personalized therapeutic delivery in the neurosurgical operating room
Q1 · CROSS-FIELD
Article
Author: Vogelbaum, Michael A.
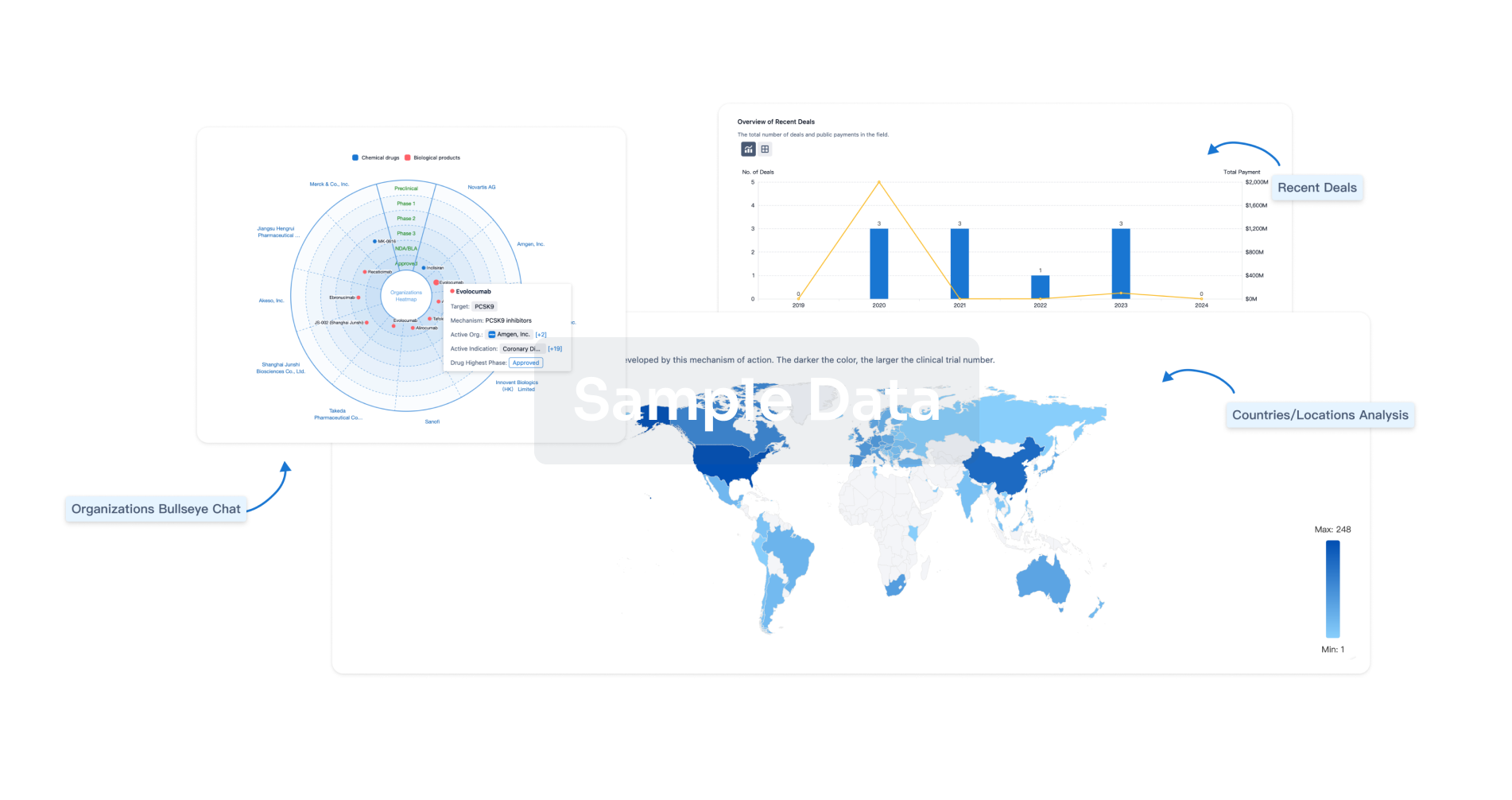
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
