Request Demo
Last update 08 May 2025
SPARCL1
Last update 08 May 2025
Basic Info
Synonyms Hevin, High endothelial venule protein, MAST 9 + [4] |
Introduction- |
Related
1
Drugs associated with SPARCL1CN116036236
Patent MiningTarget |
Mechanism- |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhaseDiscovery |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with SPARCL1
Login to view more data
100 Translational Medicine associated with SPARCL1
Login to view more data
0 Patents (Medical) associated with SPARCL1
Login to view more data
276
Literatures (Medical) associated with SPARCL101 Apr 2025·Molecular Therapy
AAV-Sparcl1 promotes hair cell regeneration by increasing supporting cell plasticity
Article
Author: Li, Nianci ; Sun, Qiuhan ; Zhou, Yinyi ; Zhang, Liyan ; Qi, Jieyu ; Zhang, Ziyu ; Tan, Fangzhi ; Ding, Xiaoqiong ; Qian, Xiaoyun ; Wang, Man ; Ye, Fanglei ; Chai, Renjie ; Lu, Yicheng
01 Apr 2025·ESC Heart Failure
SPARCL1 and NT‐proBNP as biomarkers of right ventricular‐to‐pulmonary artery uncoupling in pulmonary hypertension
Article
Author: Sossalla, Samuel ; Gall, Henning ; Richter, Manuel J. ; van Wickern, Paulina ; Liebetrau, Christoph ; Yogeswaran, Athiththan ; Nef, Holger ; Keranov, Stanislav ; Ghofrani, Ardeschir ; Dörr, Oliver ; Tello, Khodr ; Hamm, Christian ; Bauer, Pascal ; Seeger, Werner ; Troidl, Christian ; Voss, Sandra
01 Apr 2025·Stem Cell Reports
The lung microvasculature promotes alveolar type 2 cell differentiation via secreted SPARCL1
Article
Author: Cleaver, Ondine ; Kim, Hyun-Taek ; Lautenschläger, Till ; Günther, Stefan ; Alayoubi, Yousef ; Looso, Mario ; Stainier, Didier Y R ; Panza, Paolo ; Piesker, Janett
Analysis
Perform a panoramic analysis of this field.
login
or
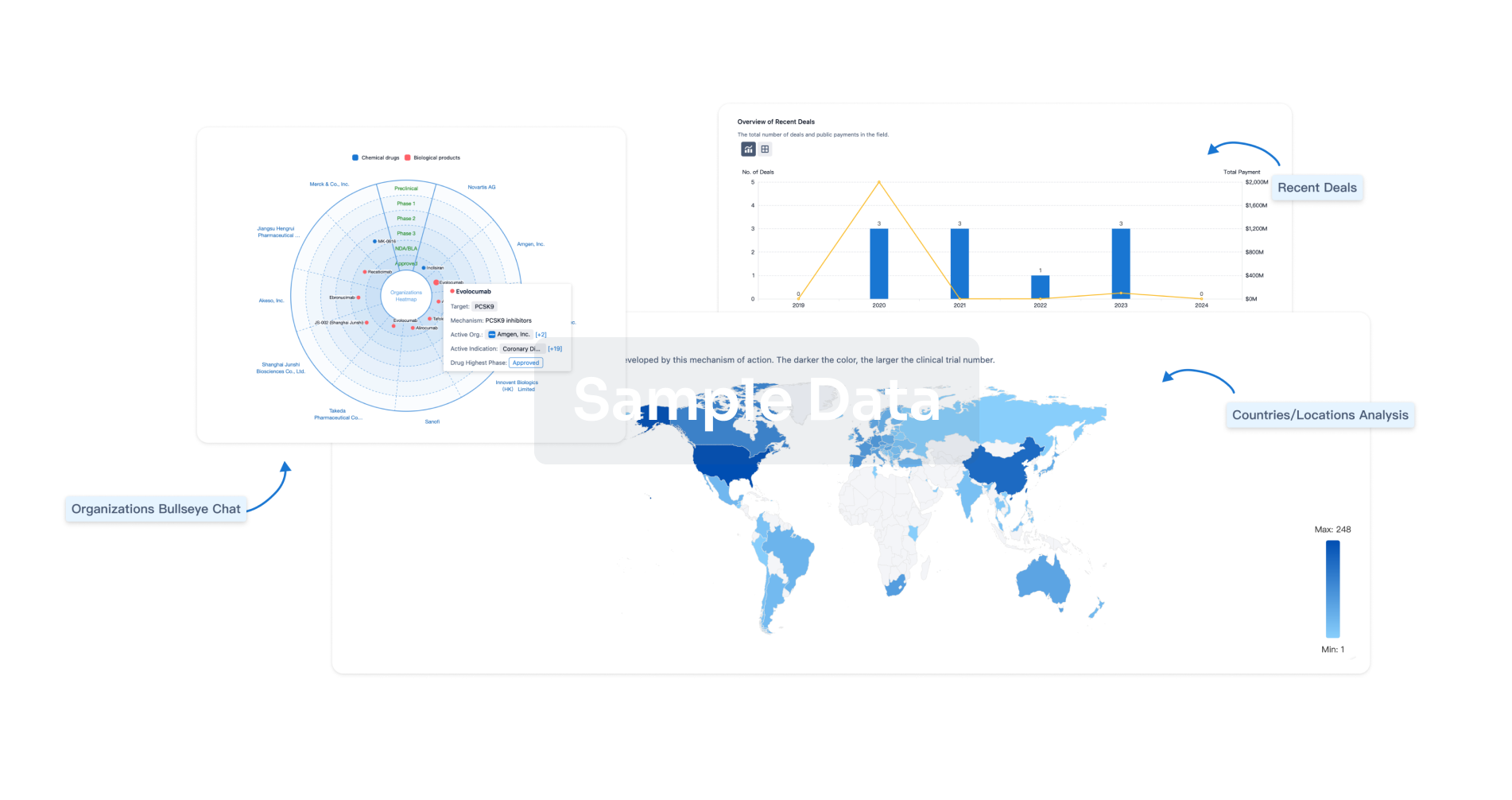
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
