Request Demo
Last update 08 May 2025
CTLA4 x PD-1 x MUC1
Last update 08 May 2025
Related
2
Drugs associated with CTLA4 x PD-1 x MUC1Mechanism CTLA4 inhibitors [+3] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism CTLA4 inhibitors [+2] |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
1
Clinical Trials associated with CTLA4 x PD-1 x MUC1NCT03179007
A Clinical Study of CTLA-4 and PD-1 Antibodies Expressing MUC1-CAR-T Cells for Patients With MUC1 Positive Advanced Solid Tumors
This is a single-arm, open-label, one center clinical study, to determine the safety and efficacy of infusion of autologous T cells engineered to express immune checkpoint antibodies (CTLA-4 and PD-1) and chimeric antigen receptor targeting MUC1 in adult patients with MUC1 positive, advanced recurrent or refractory malignant solid tumors.
Start Date07 Jun 2017 |
Sponsor / Collaborator |
100 Clinical Results associated with CTLA4 x PD-1 x MUC1
Login to view more data
100 Translational Medicine associated with CTLA4 x PD-1 x MUC1
Login to view more data
0 Patents (Medical) associated with CTLA4 x PD-1 x MUC1
Login to view more data
6
Literatures (Medical) associated with CTLA4 x PD-1 x MUC115 Dec 2015·Klinicka onkologie
Immunotherapy for the Prevention and Treatment of Breast Cancer
Review
Author: Svoboda, Marek ; Slabý, Ondřej ; Navrátil, Jiří
01 Sep 2014·Current Oncology ReportsQ2 · MEDICINE
Immunotherapeutic Agents in Non-small-cell Lung Cancer Finally Coming to the Front Lines
Q2 · MEDICINE
Review
Author: Luis E. Raez ; Rossana Ruiz ; Brian Hunis
01 Sep 2012·Annals of OncologyQ1 · MEDICINE
What future opportunities may immuno-oncology provide for improving the treatment of patients with lung cancer?
Q1 · MEDICINE
Review
Author: Reck, M
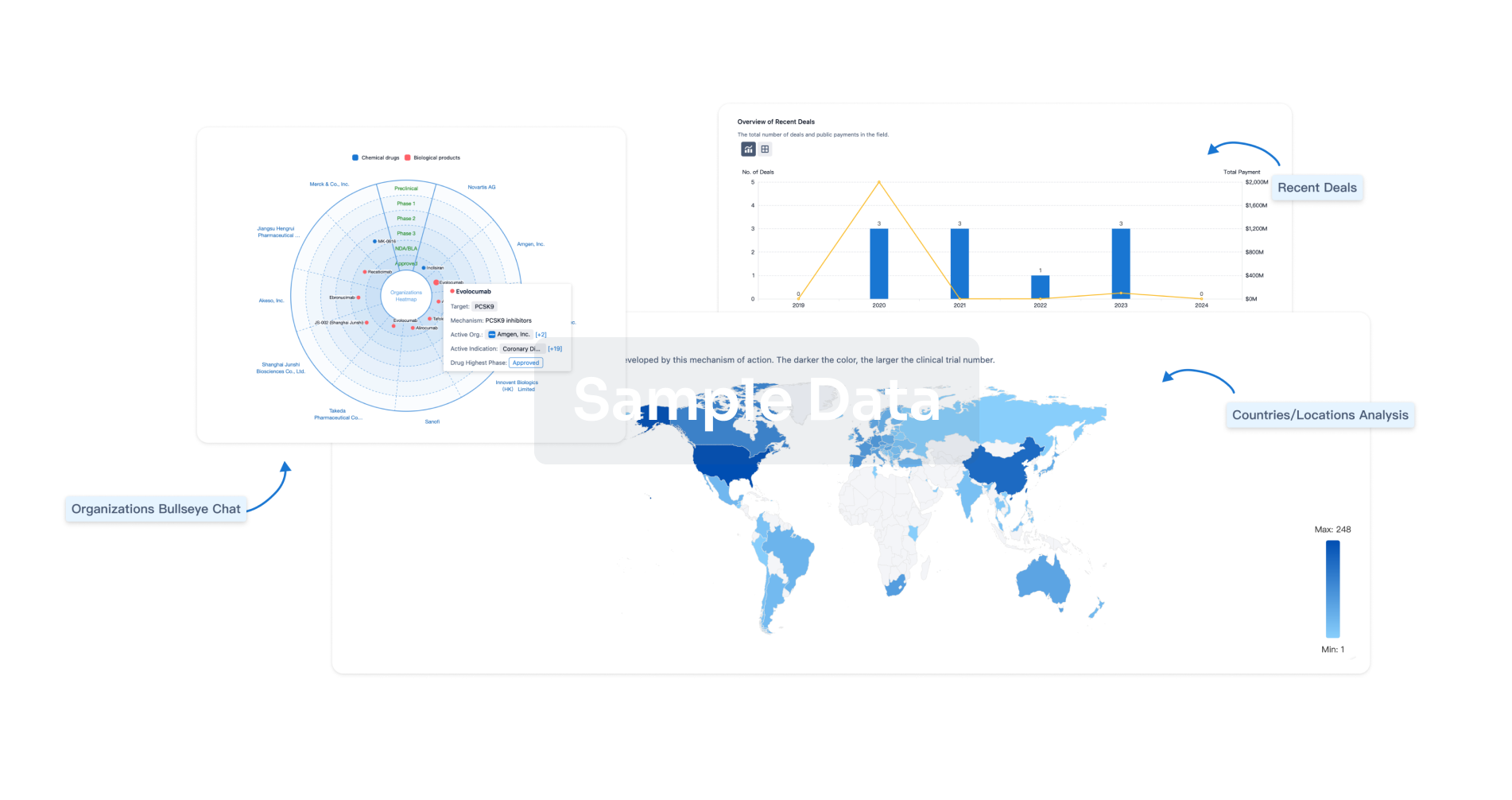
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

