Request Demo
Last update 08 May 2025
STK39 x OSR1
Last update 08 May 2025
Related
2
Drugs associated with STK39 x OSR1Target |
Mechanism OSR1 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism OSR1 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with STK39 x OSR1
Login to view more data
100 Translational Medicine associated with STK39 x OSR1
Login to view more data
0 Patents (Medical) associated with STK39 x OSR1
Login to view more data
204
Literatures (Medical) associated with STK39 x OSR103 Feb 2025·Brain
Chloride deregulation and GABA depolarization in MTOR-related malformations of cortical development
Article
Author: Huberfeld, Gilles ; Muresan, Raul C ; Blauwblomme, Thomas ; Barcia, Giulia ; Rguez, Yasmine ; Lourdel, Stéphane ; Dan, Emanuela Loredana ; Castaño-Martín, Reyes ; Guerrera, Ida Chiara ; Planelles, Gabrielle ; Bourgeois, Marie ; Asnafi, Vahid ; Chhuon, Cerina ; Kabashi, Edor ; Metais, Alice ; Lepicka, Joanna ; Balducci, Estelle ; Kaminska, Anna ; Ciura, Sorana ; Auvin, Stéphane ; Chemaly, Nicole ; Bakouh, Naziha ; Nabbout, Rima ; Losito, Emma ; Varlet, Pascale ; Moca, Vasile Vlad
01 Oct 2024·Kidney360
With No Lysine (K) Kinases and Sodium Transporter Function in Solute Exchange with Implications for BP Regulation as Elucidated through Drosophila
Review
Author: Rodan, Aylin R.
01 Sep 2024·Kidney360
Cullin 3/with No Lysine [K] Kinase/Ste20/SPS-Related Proline Alanine Rich Kinase Signaling: Impact on NaCl Cotransporter Activity in BP Regulation
Review
Author: McCormick, James A ; Omage, Kingsley
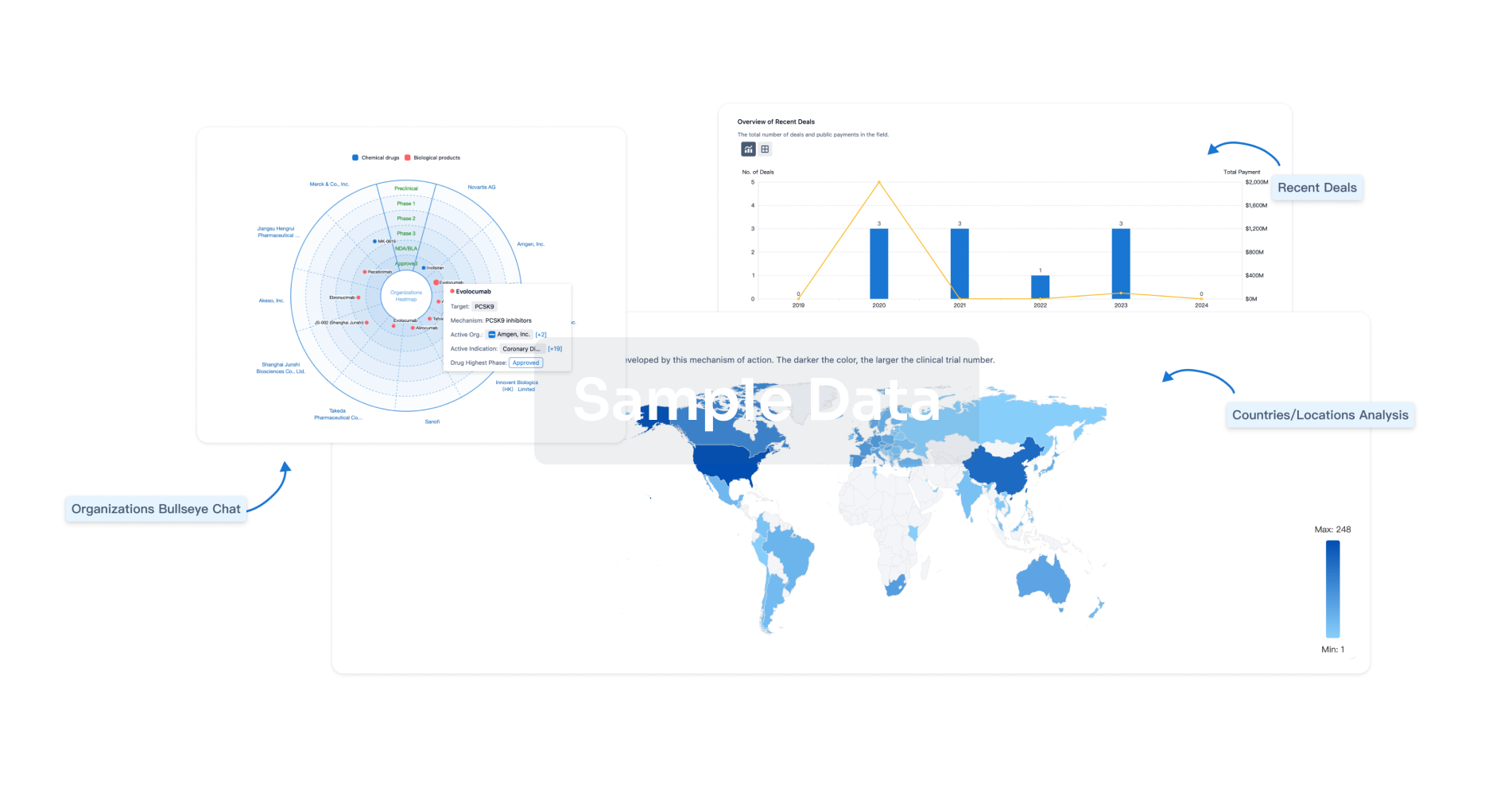
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
