Request Demo
Last update 08 May 2025
H3K9me3
Last update 08 May 2025
Basic Info
Synonyms- |
Introduction- |
Related
3
Drugs associated with H3K9me3Target |
Mechanism H3K9me3 inhibitors |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism EHMT2 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication- |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism H3K9me3 inhibitors |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with H3K9me3
Login to view more data
100 Translational Medicine associated with H3K9me3
Login to view more data
0 Patents (Medical) associated with H3K9me3
Login to view more data
2,157
Literatures (Medical) associated with H3K9me301 Sep 2025·Journal of Environmental Sciences
Carbon black induced pulmonary fibrosis through piR-713551/PIWIL4 targeting THBS2 signal pathway
Article
Author: Wang, Jingyuan ; Bao, Lei ; Pang, Yaxian ; Du, Zhe ; Niu, Yong ; Wu, Ruiting ; Wu, Mengqi ; Wang, Mengruo ; Yang, Peihao ; Zhang, Rong ; Shi, Beibei ; Liu, Qingping ; Niu, Yujie ; Chen, Jiawei
01 Jul 2025·European Journal of Pharmacology
Irisin attenuates liver fibrosis by regulating energy metabolism and HMGB1/β-catenin signaling in hepatic stellate cells
Article
Author: Wang, Xu ; Hou, Minna ; He, Qi ; Li, Jing ; Liu, Yunting ; Hou, Yali ; Li, Ying ; Bai, Ning ; Liu, Xin ; Li, Fang
01 Jun 2025·Non-coding RNA Research
Long noncoding RNA hottip maintained skeletal homeostasis via suppressing the enhancer of zeste homolog 2 (Ezh2)/histone methylation regulatory axis
Article
Author: Zhou, Shu-Ting ; Liang, Wei-Cheng ; Shi, Chuan-Jian ; Liang, Pu-Ping ; Mai, Yong-Xin ; Shao, Jiang ; Zhang, Jin-Fang ; Li, Zhi-Peng
1
News (Medical) associated with H3K9me302 May 2024
Discovery led by experts at Cincinnati Children's reveals potential treatment for multiple sclerosis (MS), age-related cognitive deficits, and other rare neural diseases
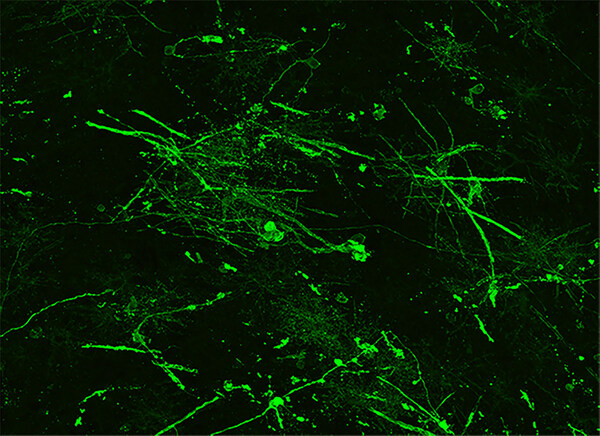
CINCINNATI, May 2, 2024 /PRNewswire/ -- When treated with a novel protein function inhibitor called ESI1, mice that mimic the symptoms of multiple sclerosis (MS) and lab-prepared human brain cells both demonstrated the ability to regenerate vital myelin coatings that protect healthy axon function.
This breakthrough, published May 2, 2024, in Cell, appears to overcome difficulties that have long frustrated previous attempts to reverse a form of nerve damage that robs people with MS of motor control and gradually blunts cognitive functions for many people as they age.
Continue Reading
In human organoid cells, ESI1 treatment strengthened myelin sheath production, as shown by the thick, long green strands. in this confocal microscope image.
"Currently, there are no effective therapies to reverse myelin damage in devastating demyelinating diseases such as MS," says corresponding author Q. Richard Lu, PhD, a top brain research expert at Cincinnati Children's. "These findings are significant as they offer new pathways for treatment that potentially shift the therapeutic focus from just managing symptoms to actively promoting repair and regeneration of myelin."
Promoting healing by clearing a roadblock
A critical insight driving the new findings was observing that brain regions damaged by MS still possessed a type of cell needed to repair myelin damage, but the disease activates other cell types and signals that combine forces to silence the repair function.
These useful cells in the brain, called oligodendrocytes, are responsible for producing myelin sheaths that wrap around cable-like parts of nerve cells called axons, much like the plastic insulation around a wire. When the protective myelin gets damaged, be it by disease or the wear and tear of age, nerve signaling gets disrupted. Depending on where the damaged nerves lead, the disruptions can affect movement, vision, thinking and so on.
Essentially, the research team found a way to unsilence the silenced repair process, setting the oligodendrocytes (OLs) free to do their jobs.
Pinning down the genetic changes and signals involved in the repair silencing process and finding a small molecule compound that can reverse the silencing was a complex undertaking. The project, which spanned over five years, involved four co-first authors and 29 contributing co-authors from Cincinnati Children's, the University of Cincinnati, and 14 other institutions including universities in Australia, China, Germany, India, Singapore, and the United Kingdom.
Among the team's key findings:
Identifying the mechanism preventing myelin production in MS
Analysis of stored autopsy tissues revealed that OLs within MS lesions lacked an activating histone mark called H3K27ac, while expressing high levels of two other repressive histone marks H3K27me3 and H3K9me3 associated with silencing gene activity.
Finding a compound that can reverse the silencing
The research team scoured a library of hundreds of small molecules known to target enzymes that could modify gene expression and influence the silenced OLs. The team determined that the compound ESI1 (epigenetic-silencing-inhibitor-1) was nearly five times more powerful than any other compounds they considered.
The compound tripled the levels of the desired H3K27ac histone mark in OLs while sharply reducing levels of the two repressive histone marks. Additionally, the research reveals a new way in which ESI1 promotes the creation of special membrane-less regulatory hubs known as "biomolecular condensates" within the cell nucleus that control fat and cholesterol levels. These hubs act as central points to boost the production of essential fats and cholesterol needed to make myelin, a crucial component of nerve fibers.
Demonstrating benefits in mice and lab-grown human tissue
In both aging mice and mice mimicking MS, the ESI1 treatment prompted myelin sheath production and improved lost neurological function. Testing included tracking gene activation, measuring the microscopic new myelin sheaths surrounding axons, and observing that treated mice were quicker at navigating a water maze.
Then the team tested the treatment on lab-grown human brain cells. The team used a type of brain organoid, myelin organoids, that is far more simplified than a full brain but still produces complex myelinating cells. When the organoids were exposed to ESI1, the treatment extended the myelin sheath of myelinating cells, the study reports.
Implications and next steps
MS is the most common and best known of several major neurodegenerative diseases. The new findings may spark a new approach to stopping the degenerative effects of these conditions, Lu says.
Myelin regeneration treatment also could be helpful for people recovering from brain and spinal cord injuries.
But the most far-reaching implication of the study is the possibility of using ESI1, or similar compounds, to help slow or even reverse cognitive losses that often occur during aging. Many studies have shown that myelin loss plays a role in age-related loss of cognitive function, Lu says.
However, more research is needed to determine whether human clinical trials can be launched to evaluate ESI1 as a potential treatment. For example, the effects of ESI1 may need to be modulated by adjusting the dose, treatment duration, or using "pulsed therapy" during specific time windows. More study also is needed to determine whether even more effective compounds than ESI1 might be designed from scratch.
"This study is a beginning," Lu says. "Prior to finding ESI1, most scientists believed that remyelination failure in MS was due to the stalled development of precursors. Now we show a proof of concept that reversing the silencing activity in OLs present in the damaged brain can enable myelin regeneration."
About the study
These researchers contributed equally as co-first authors: Xuezhao Liu, Dazhuan Eric Xin, Xiaowen Zhong and Chuntao Zhao, all with Cincinnati Children's. Xuelian He, of West China Second University Hospital, Sichuan, China, was a co-corresponding author.
Co-authors from Cincinnati Children's included Liguo Zhang, Arman Bayat, Eva Nicholson, William Seibel, Mei Xin, Adam Dourson, Jason Tchieu, and Michael Jankowski. Bingfang Yan, of the Division of Pharmaceutical Sciences at the University of Cincinnati also contributed.
Funding sources for this study include the National Multiple Sclerosis Society and the National Institutes of Health (R01NS113965, R01NS105715, R01AA030486, R01AI172959, and R35NS097303) and the National Key R&D Program of China (2022YFA1105500). The authors declare no conflict of interest.
SOURCE Cincinnati Children's Hospital Medical Center
Clinical Result
Analysis
Perform a panoramic analysis of this field.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free