Request Demo
Last update 23 Jan 2025
IL-3 x CD molecules x Fibronectin type III domain containing
Last update 23 Jan 2025
Basic Info
Related Targets |
Related
1
Drugs associated with IL-3 x CD molecules x Fibronectin type III domain containingUS20240024479
Patent MiningMechanism- |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhaseDiscovery |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with IL-3 x CD molecules x Fibronectin type III domain containing
Login to view more data
100 Translational Medicine associated with IL-3 x CD molecules x Fibronectin type III domain containing
Login to view more data
0 Patents (Medical) associated with IL-3 x CD molecules x Fibronectin type III domain containing
Login to view more data
574
Literatures (Medical) associated with IL-3 x CD molecules x Fibronectin type III domain containing01 Jan 2025·Ecotoxicology and Environmental Safety
Podophyllotoxin mediates hepatic toxicity via the C5a/C5aR/ROS/NLRP3 and cGMP/PKG/mTOR axis in rats based on toxicological evidence chain (TEC) concept by phosphoproteomic analysis
Article
Author: Liu, Chuanxin ; Huang, Xiaobin ; Zhang, Fangfang ; Duan, Jiajia ; Wang, Yuming ; Kong, Jiao ; Li, Xuejiao
01 Jan 2025·Immunological Reviews
The β Common Cytokine Receptor Family Reveals New Functional Paradigms From Structural Complexities
Review
Author: Yip, Kwok Ho ; Kan, Winnie L. ; Liu, Nora W. ; Thomas, Daniel ; Woodcock, Joanna M. ; Tvorogov, Denis ; Owczarek, Catherine M. ; Hercus, Timothy R. ; Tumes, Damon J. ; Parker, Michael W. ; Nero, Tracy L. ; Ross, David M. ; Pant, Harshita ; Terán, David ; Lopez, Angel F. ; Martelotto, Luciano G. ; Polo, Jose M. ; Weekley, Claire M.
01 Oct 2024·Journal for ImmunoTherapy of Cancer
NSGS mice humanized with cord blood mononuclear cells show sustained and functional myeloid–lymphoid representation with limited graft-versus-host disease
Article
Author: Pradenas, Edwards ; Lázaro-Díez, María ; Prado, Julia G ; Roca Ho, Heleia ; Carcaboso, Ángel M ; Blanco, Julià ; Falgas, Aida ; Martinez-Moreno, Alba ; González-Navarro, Europa Azucena ; Menendez, Pablo ; Juan, Manel ; Carabelli, Julieta ; Panisello, Carla ; Bueno, Clara ; Carrillo, Jorge ; Aschero, Rosario
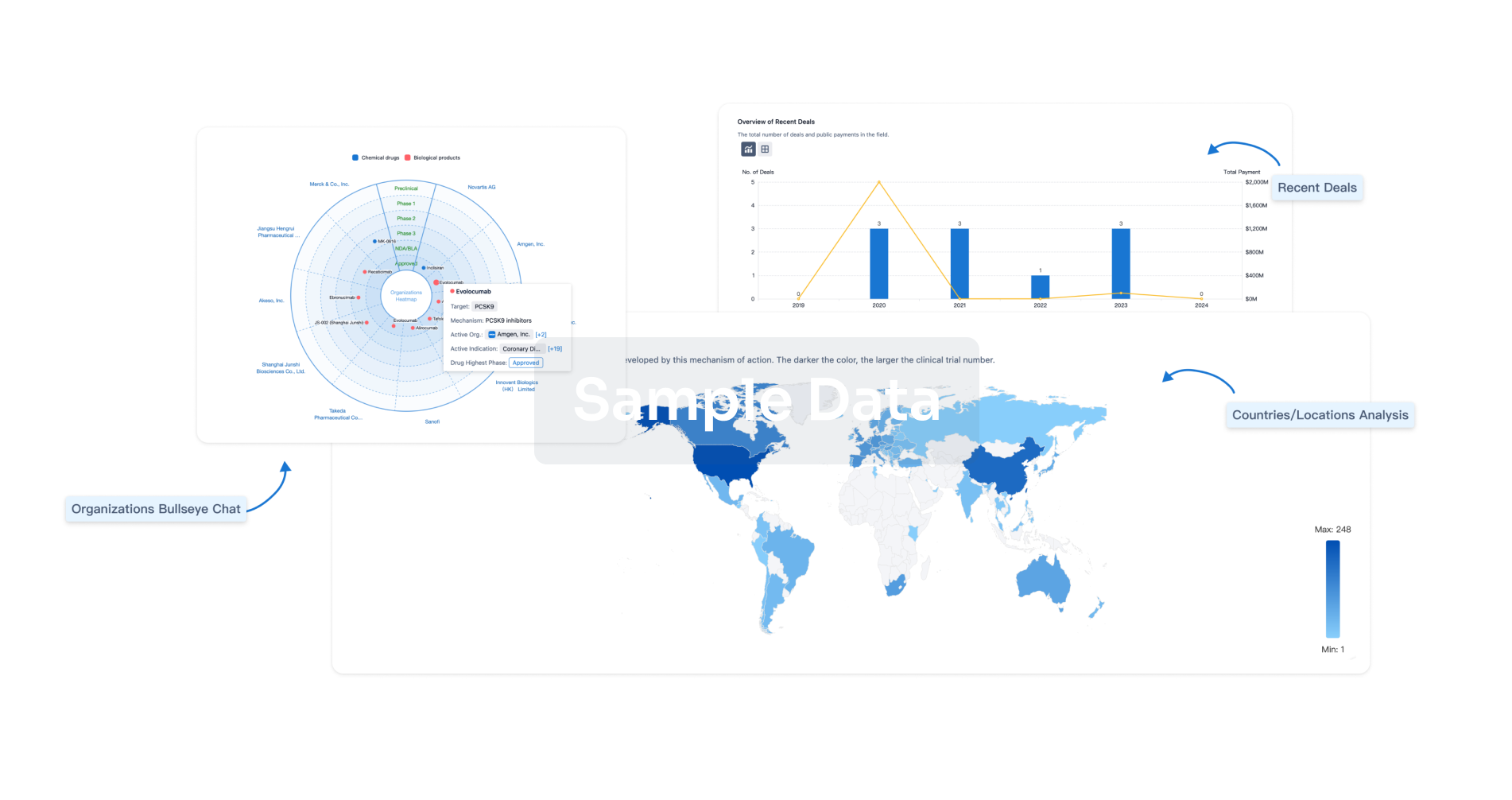
Analysis
Perform a panoramic analysis of this field.
login
or
Chat with Hiro
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
