Request Demo
Last update 08 May 2025
TRH x TSHR x TRHR
Last update 08 May 2025
Related
1
Drugs associated with TRH x TSHR x TRHRTarget |
Mechanism TRH agonists [+2] |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhaseDiscontinued |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with TRH x TSHR x TRHR
Login to view more data
100 Translational Medicine associated with TRH x TSHR x TRHR
Login to view more data
0 Patents (Medical) associated with TRH x TSHR x TRHR
Login to view more data
493
Literatures (Medical) associated with TRH x TSHR x TRHR26 Nov 2024·Journal of the Endocrine Society
Role of Thyrotropin-Releasing Hormone Stimulation Test and Autoantibody in 952 Subjects with Subclinical Hypothyroidism
Article
Author: Byun, Dong Won ; Park, Sang Joon ; Park, Hyeong Kyu ; Suh, Kyoil ; Yoo, Myung Hi ; Kim, Hye Jeong ; Park, Suyeon
30 Apr 2024·Endocrinology and Metabolism
Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
Article
Author: Kong, Doo-Sik ; Kim, Se Hoon ; Jin, Sang-Man ; Nam, Do-Hyun ; Lee, Won-Jae ; Kim, Gyuri ; Hong, Sang Duk ; Suh, Yeon-Lim ; Hur, Kyu Yeon ; Kim, Sung Tae ; Lee, You-Bin ; Ryu, Sujin ; Kim, Jae Hyeon ; Heo, Jung
01 Aug 2023·Development, growth & differentiation
Hormonal and pheromonal studies on amphibians with special reference to metamorphosis and reproductive behavior.
Review
Author: Kikuyama, Sakae ; Toyoda, Fumiyo ; Kouki, Tom ; Yamamoto, Kazutoshi ; Okada, Reiko
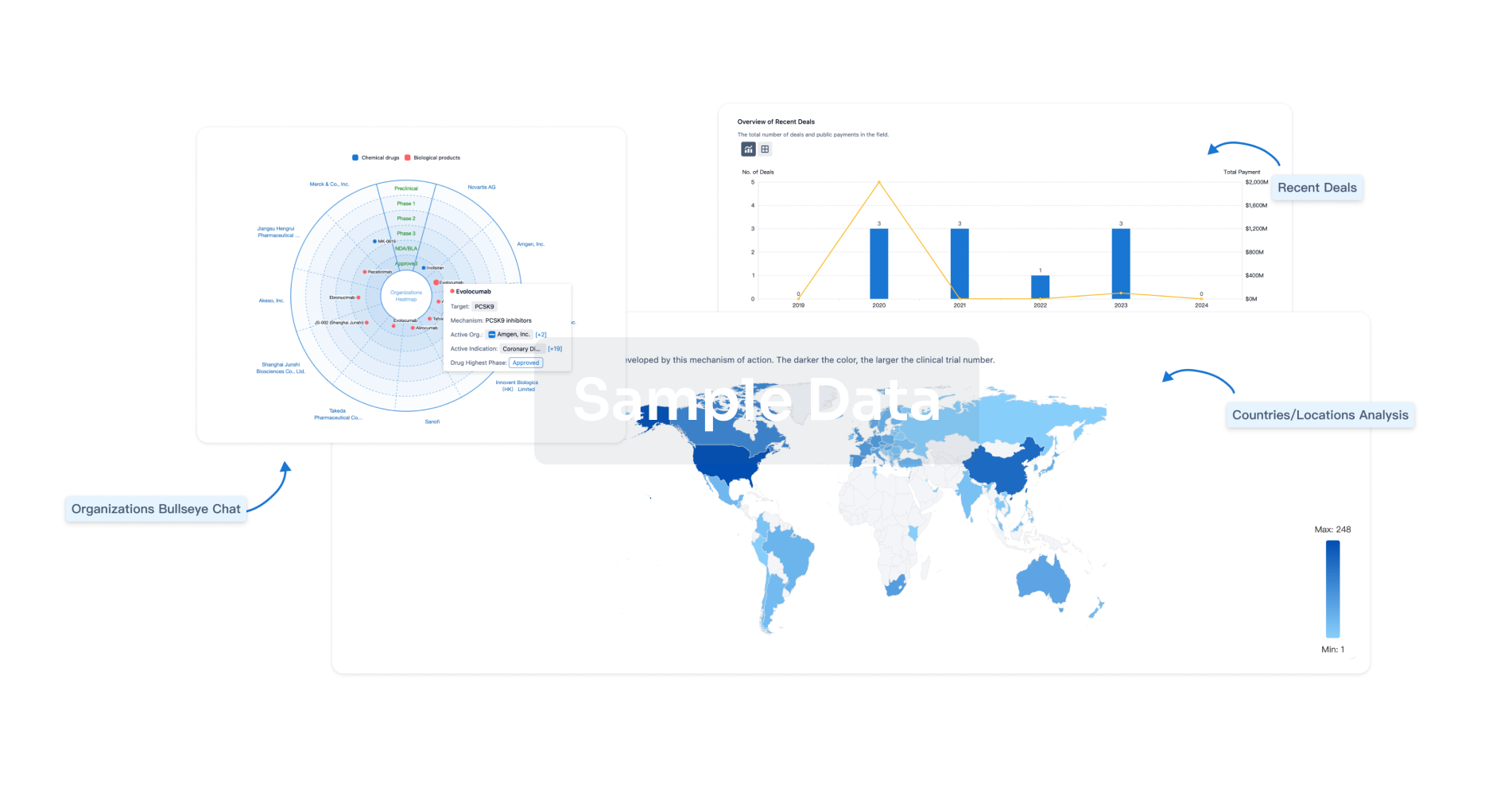
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free