Request Demo
Last update 08 May 2025
MCPyV
Last update 08 May 2025
Basic Info
Synonyms MCPyV蛋白 |
Introduction- |
Related
1
Drugs associated with MCPyVTarget |
Mechanism MCPyV antagonists |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with MCPyV
Login to view more data
100 Translational Medicine associated with MCPyV
Login to view more data
0 Patents (Medical) associated with MCPyV
Login to view more data
244
Literatures (Medical) associated with MCPyV01 Dec 2025·Endocrine Pathology
Evaluating CK20 and MCPyV Antibody Clones in Diagnosing Merkel Cell Carcinoma
Article
Author: Ozluk, Yasemin ; Kozanoglu, Erol ; Yeni Erdem, Begum ; Buyukbabani, Nesimi ; Baykal, Can ; Ozturk Sari, Sule ; Ahmed, Melin A ; Saip, Pinar
01 May 2025·The American Journal of Dermatopathology
NSD3::FGFR1: A Novel Gene Fusion First to Be Described in Merkel Cell Carcinoma
Article
Author: Lenskaya, Volha ; Yang, Richard K ; Prieto, Victor G ; Nagarajan, Priyadharsini ; Aung, Phyu P ; Cho, Woo Cheal
01 Apr 2025·Pathology
Merkel cell carcinoma in Taiwan: a subset is chronic arsenicism-related, and the Merkel cell polyomavirus-negative cases are pathologically distinct from virus-related cases with a poorer outcome
Article
Author: Lai, Yun-Ru ; Chuang, Shih-Sung ; Yu, Wei-Wen ; Cheng, Pai-Shan ; Wang, Ren Ching ; Liu, Chih-Yi ; Shen, Wan-Lin
4
News (Medical) associated with MCPyV23 Oct 2023
ITI-3000 Demonstrated a Favorable Safety and Tolerability Pro >
Patients showed encouraging immunological responses, which will be further confirmed with a Phase II trial
ROCKVILLE, Md.--(BUSINESS WIRE)--Immunomic Therapeutics, Inc. (ITI), a privately-held clinical-stage biotechnology company pioneering the development of LAMP-mediated nucleic acid-based immunotherapy, today announced safety and tolerability results from its phase 1 clinical trial evaluating ITI-3000, a plasmid DNA (pDNA) vaccine, targeting patients with Merkel cell carcinoma (MCC), a rare but aggressive form of skin cancer that is typically caused by the Merkel cell polyomavirus (MCPyV). ITI-3000 was granted Fast Track Designation (FTD) by the U.S. Food and Drug Administration (FDA) in November 2022.
"The reporting of results from our phase 1 trial of ITI-3000 in patients with MCC, marks the achievement of a significant milestone in our mission to create a therapeutic solution for this rare, yet highly aggressive skin cancer," stated D.G. Kim, Chief Executive Officer of ITI. "As we expected, ITI-3000 proved to be safe and well tolerated in the study, with no dose-limiting toxicities, no reported treatment-related adverse events or serious adverse reactions. As we are encouraged by the immunological responses in patients, we look forward to continuing the development of ITI-3000. The advancement of this program is paving the way for the expansion of our pipeline via our UNITE® platform."
The phase 1 clinical trial was a six-patient, single center, open label, first-in-human (FIH) study, investigating the safety, tolerability and immunogenicity of ITI-3000 in patients with polyomavirus-positive Merkel cell carcinoma (MCC). Participants received 4 doses of ITI-3000 vaccine, one 4 mg dose every month for four months. Participants in the study were those who are both diagnosed and had completed standard of care (SOC) surgical and/or radiation therapy at least one year prior to enrollment in the study, and who had no evidence of active disease (NEAD). Participants who were previously diagnosed with MCC and had recurrence but exhibited no evidence of active disease (NEAD) for more than two years prior to enrollment, were also included in the study.
Additional information regarding the phase 1 trial may be found at clinicaltrials.gov, using identifier: NCT05422781.
About ITI-3000
ITI-3000 leverages the company’s investigational UNiversal Intracellular Targeted Expression (UNITE®) platform, powered by LAMP (Lysosome Associated Membrane Protein), which fuses sequences from the mutated form of the large T antigen (LT) of the MCPyV into the sequence of the LAMP-1 gene. This lysosomal targeting technology has been shown to result in enhanced antigen presentation and a potent immune response.
About Immunomic Therapeutics, Inc.
Immunomic Therapeutics, Inc. (ITI) is a privately-held, clinical-stage biotechnology company pioneering the development of vaccines through its proprietary technology platform UNITE®, which is designed to utilize the body’s natural biochemistry to develop vaccines that generate broad immune responses. ITI is primarily focused on applying the UNITE platform to oncology indications, where it could potentially have broad applications, including development of antigen-derived antibodies as biologics in a number of cancers. The company has built a pipeline leveraging UNITE with programs in oncology, animal health, infectious disease, and allergy. ITI maintains its headquarters in Rockville, Maryland. For more information, please visit .
Forward-Looking Statements
This press release includes statements relating to the current progress of the ITI-3000 program for Merkel cell carcinoma and ITI’s technology platform and development efforts. These statements and other statements regarding our future plans and goals constitute "forward-looking statements" and are intended to qualify for the safe harbor from liability established by the Private Securities Litigation Reform Act of 1995. Such statements are subject to risks and uncertainties that are often difficult to predict, are beyond our control and which may cause results to differ materially from expectations, including, without limitation, whether we are able to capitalize on the Fast Track Designation for the ITI-3000 program, receive additional accelerated review from the FDA, achieve positive results in our clinical trials to develop an immunotherapy that is successful in treating MCC, and be able to advance the utilization of our UNITE® platform. You are cautioned not to place undue reliance on these forward-looking statements, which are based on our expectations as of the date of this press release and speak only as of the origination date of this press release. We undertake no obligation to publicly update or revise any forward-looking statement, whether as a result of new information, future events or otherwise.
Clinical ResultFast TrackVaccinePhase 1Immunotherapy
08 Nov 2022
ROCKVILLE, Md.--(BUSINESS WIRE)-- Immunomic Therapeutics, Inc. (ITI), a privately-held clinical-stage biotechnology company pioneering the development of LAMP-mediated nucleic acid-based immunotherapy, today announced that the U.S. Food and Drug Administration (FDA) has granted Fast Track Designation (FTD) to the ITI-3000 program for the treatment of patients with Merkel cell carcinoma. The company is currently enrolling a phase 1 study evaluating ITI-3000, a plasmid DNA (pDNA) vaccine targeting patients with Merkel cell carcinoma (MCC), a rare but aggressive form of skin cancer that is typically caused by the Merkel cell polyomavirus (MCPyV).
“The FDA’s decision to grant FTD underscores the potential for the ITI-3000 program to address a serious unmet need and serve as a meaningful therapeutic option for patients with Merkel cell carcinoma,” stated Dr. William Hearl, Chief Executive Officer of ITI. “We are committed to unlocking the full potential of ITI-3000 in patients with this aggressive form of skin cancer. We expect to report top-line data from our ongoing phase 1 trial of ITI-3000 in MCC patients next year and look forward to working closely with the FDA on a potential next phase clinical study design, while simultaneously continuing dialogue with possible partners.”
ITI-3000 leverages the company’s investigational UNiversal Intracellular Targeted Expression (UNITE®) platform, powered by LAMP (Lysosome Associated Membrane Protein), which fuses sequences from the mutated form of the large T antigen (LT) of the MCPyV into the sequence of the LAMP-1 gene. This lysosomal targeting technology has been shown to result in enhanced antigen presentation and a balanced immune response, including, of note, ITI-3000 activated antigen-specific CD4+ T cells in vivo.
About Fast Track Designation
Fast Track Designation is designed to facilitate the development and expedite the FDA review of drugs to treat serious conditions and fulfill unmet medical needs, enabling drugs to reach patients earlier. Clinical programs with Fast Track Designation benefit from early and frequent communication with the FDA throughout the regulatory review process. These clinical programs may also be eligible to apply for accelerated approval and breakthrough designation review by the FDA if relevant criteria are met.
About UNITE®
ITI’s UNITE platform leverages the ability to engineer chimeric proteins, directing antigen presenting cells to present antigens to the immune system through a targeted pathway and driving a robust immune response. UNITE vaccines are distinct in that they combine two components: nucleic acid constructs that encode a specific antigen and an endogenous Lysosomal Associated Membrane Protein (LAMP-1) sequence. The UNITE platform harnesses LAMP-1 as a means of presenting the vaccine target to the immune system, resulting in antibody production, inflammatory cytokine release, and establishing critical immunological memory, something that other vaccine approaches commonly lack. This approach could put UNITE technology at the crossroads of immunotherapies in multiple indications, including cancer, human allergy, animal health, and infectious disease. Preclinical data is currently being developed to explore whether LAMP-1 nucleic acid constructs may amplify and activate the immune response in highly immunogenic tumor types and be used to create immune responses in tumor types that otherwise do not provoke an immune response.
About Immunomic Therapeutics, Inc.
Immunomic Therapeutics, Inc. (ITI) is a privately-held, clinical-stage biotechnology company pioneering the development of vaccines through its proprietary technology platform UNITE, which is designed to utilize the body’s natural biochemistry to develop vaccines that generate broad immune responses. ITI is primarily focused on applying the UNITE platform to oncology indications, where it could potentially have broad applications, including development of antigen-derived antibodies as biologics in a number of cancers. The company has built a pipeline leveraging UNITE with programs in oncology, animal health, infectious disease, and allergy. ITI maintains its headquarters in Rockville, Maryland. For more information, please visit .
Forward-Looking Statements
This press release includes statements relating to the current progress of the ITI-3000 program for Merkel cell carcinoma and ITI’s technology platform and development efforts. These statements and other statements regarding our future plans and goals constitute "forward-looking statements" and are intended to qualify for the safe harbor from liability established by the Private Securities Litigation Reform Act of 1995. Such statements are subject to risks and uncertainties that are often difficult to predict, are beyond our control and which may cause results to differ materially from expectations, including, without limitation, whether we are able to capitalize on the Fast Track Designation for the ITI-3000 program, receive additional accelerated review from the FDA, achieve positive results in our clinical trials to develop an immunotherapy that is successful in treating MCC, and be able to advance the utilization of our UNITE platform. You are cautioned not to place undue reliance on these forward-looking statements, which are based on our expectations as of the date of this press release and speak only as of the origination date of this press release. We undertake no obligation to publicly update or revise any forward-looking statement, whether as a result of new information, future events or otherwise.
VaccineCollaborateAntibodyImmunotherapyFast Track
20 Jul 2022
July 20, 2022 11:00 UTC
-Top line data expected in second half of 2023-
ROCKVILLE, Md.--(BUSINESS WIRE)--Immunomic Therapeutics, Inc., (“ITI”), a privately-held clinical-stage biotechnology company pioneering the study of LAMP (Lysosome Associated Membrane Protein)-mediated nucleic acid-based immunotherapy, today announced dosing of the first patient in the company’s Phase 1 study evaluating ITI-3000, a plasmid DNA (pDNA) vaccine targeting patients with Merkel cell carcinoma (MCC), a rare but aggressive form of skin cancer that is typically caused by the Merkel cell polyomavirus (MCPyV). The single-center study is being conducted at the University of Washington School of Medicine and the Fred Hutchinson Cancer Center in Seattle, Washington and is being led by Drs. Paul Nghiem, Song Park and David M. Koelle.
The eight-patient, open label, first-in-humans (FIH) study is designed to evaluate the safety, tolerability, and immunogenicity of 4 mg of ITI-3000 in patients with MCC who have undergone surgery. The study’s primary endpoints include the number of participants experiencing dose limiting toxicities (DLTs), the number of occurrences of adverse events/serious adverse reactions, (AEs/SARs), as well as other standard clinical assessments and safety laboratory parameters.
ITI-3000 leverages the company’s investigational UNiversal Intracellular Targeted Expression (UNITE®) platform, powered by LAMP, which fuses sequences from the mutated form of the large T antigen (LT) of the MCPyV into the sequence of the LAMP-1 gene. This lysosomal targeting technology has been shown to result in enhanced antigen presentation and a balanced immune response, including, of note, ITI-3000 activated antigen-specific CD4+ T cells in vivo.
“Despite recent advances in cancer immunotherapy, there remains a need for therapies to treat this rather rare, but aggressive form of skin cancer, and we believe that our proprietary approach, utilizing nucleic acid vaccines with the power to leverage the body’s natural biochemistry to develop a broad immune response, holds tremendous potential in this indication,” said Dr. William Hearl, Chief Executive Officer of Immunomic Therapeutics. “We look forward to reporting top-line results from the Phase 1 trial in the second quarter of next year.”
Additional information regarding the Phase 1 trial may be found at clinicaltrials.gov, using identifier: NCT05422781.
About Immunomic Therapeutics, Inc.
Immunomic Therapeutics, Inc. (ITI) is a privately held, clinical stage biotechnology company pioneering the development of vaccines through its proprietary technology platform, UNiversal Intracellular Targeted Expression (UNITE®), which is designed to utilize the body’s natural biochemistry to develop vaccines that generate broad immune responses. UNITE® has a robust history of applications in various therapeutic areas, including infectious diseases, oncology, allergy, and autoimmune diseases. ITI is primarily focused on applying the UNITE® platform to oncology, where it could potentially have broad applications, including antigen-derived antibodies as biologics. The Company has built a pipeline leveraging UNITE® with programs in oncology, animal health, infectious disease, and allergy. ITI maintains its headquarters in Rockville, Maryland. For more information, please visit .
VaccineCollaborateAntibodyImmunotherapy
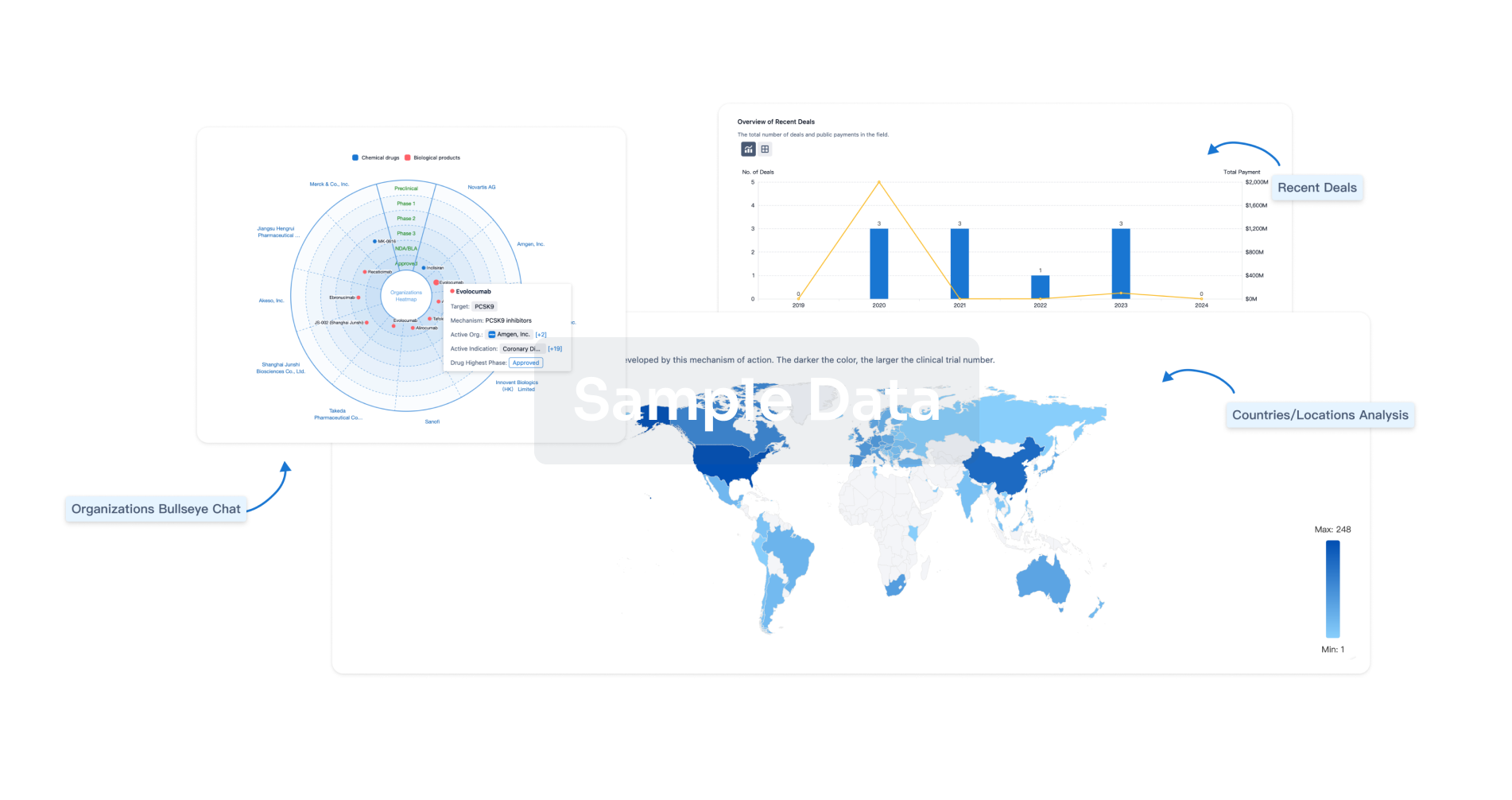
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
