Request Demo
What are TcdA inhibitors and how do they work?
25 June 2024
Clostridioides difficile, often abbreviated as C. difficile, is a bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon. The virulence of C. difficile is primarily attributed to its production of toxins, particularly TcdA (toxin A) and TcdB (toxin B). These toxins disrupt the normal functioning of cells lining the gut, leading to inflammation and tissue damage. While much attention has been given to TcdB due to its potent cytotoxicity, TcdA also plays a crucial role in the pathogenesis of C. difficile infections (CDI). This has led to an increasing interest in the development of TcdA inhibitors as a therapeutic strategy.
TcdA inhibitors work by specifically targeting the toxin A molecule, thereby neutralizing its harmful effects on the host's gut cells. TcdA is a large glycosyltransferase that modifies small GTPases in host cells, leading to the disruption of the actin cytoskeleton. This disruption results in cell rounding, loss of cell-to-cell junctions, and ultimately cell death. TcdA inhibitors are designed to block these biochemical interactions, thereby preventing the cytopathic effects that contribute to the symptoms of CDI.
There are several mechanisms by which TcdA inhibitors can achieve this blockade. One approach involves small molecules that can bind directly to the active site of TcdA, inhibiting its enzymatic activity. Another strategy is the use of monoclonal antibodies that recognize and bind to specific epitopes on TcdA, thereby preventing the toxin from interacting with its cellular targets. Research is also exploring the use of small interfering RNAs (siRNAs) to downregulate the expression of TcdA in the bacteria, though this approach is still in its experimental stages.
TcdA inhibitors are primarily used for the treatment of CDI. Currently, the standard treatment for CDI involves antibiotics like metronidazole, vancomycin, or fidaxomicin. However, these antibiotics are not always effective, and recurrence rates are high. TcdA inhibitors offer a targeted approach that could complement or even replace traditional antibiotic therapies. By specifically neutralizing one of the primary virulence factors of C. difficile, TcdA inhibitors can mitigate the symptoms of the infection without disrupting the broader microbiome. This is particularly important given that antibiotic treatment can further disrupt the gut microbiota, potentially leading to recurrent infections.
Beyond treating active infections, TcdA inhibitors also show promise in preventing recurrent CDI. Recurrent infections are a significant challenge in managing CDI, with some patients experiencing multiple relapses. The ability of TcdA inhibitors to specifically target and neutralize toxin A can reduce the likelihood of recurrence, offering a more sustainable long-term treatment strategy.
Moreover, TcdA inhibitors could have broader applications in managing other diseases influenced by similar bacterial toxins. For instance, other pathogenic bacteria produce toxins with mechanisms of action similar to TcdA. Understanding the effectiveness of TcdA inhibitors could pave the way for the development of inhibitors for these other toxins, broadening the scope of treatment options for various toxin-mediated diseases.
In conclusion, TcdA inhibitors represent a promising advancement in the treatment of Clostridioides difficile infections. By specifically targeting the toxin A molecule, these inhibitors offer a targeted approach that can mitigate the symptoms of CDI, reduce recurrence rates, and potentially offer new treatment avenues for other toxin-mediated diseases. As research continues to advance, the hope is that TcdA inhibitors will become an integral part of the therapeutic arsenal against C. difficile and other pathogenic bacteria.
TcdA inhibitors work by specifically targeting the toxin A molecule, thereby neutralizing its harmful effects on the host's gut cells. TcdA is a large glycosyltransferase that modifies small GTPases in host cells, leading to the disruption of the actin cytoskeleton. This disruption results in cell rounding, loss of cell-to-cell junctions, and ultimately cell death. TcdA inhibitors are designed to block these biochemical interactions, thereby preventing the cytopathic effects that contribute to the symptoms of CDI.
There are several mechanisms by which TcdA inhibitors can achieve this blockade. One approach involves small molecules that can bind directly to the active site of TcdA, inhibiting its enzymatic activity. Another strategy is the use of monoclonal antibodies that recognize and bind to specific epitopes on TcdA, thereby preventing the toxin from interacting with its cellular targets. Research is also exploring the use of small interfering RNAs (siRNAs) to downregulate the expression of TcdA in the bacteria, though this approach is still in its experimental stages.
TcdA inhibitors are primarily used for the treatment of CDI. Currently, the standard treatment for CDI involves antibiotics like metronidazole, vancomycin, or fidaxomicin. However, these antibiotics are not always effective, and recurrence rates are high. TcdA inhibitors offer a targeted approach that could complement or even replace traditional antibiotic therapies. By specifically neutralizing one of the primary virulence factors of C. difficile, TcdA inhibitors can mitigate the symptoms of the infection without disrupting the broader microbiome. This is particularly important given that antibiotic treatment can further disrupt the gut microbiota, potentially leading to recurrent infections.
Beyond treating active infections, TcdA inhibitors also show promise in preventing recurrent CDI. Recurrent infections are a significant challenge in managing CDI, with some patients experiencing multiple relapses. The ability of TcdA inhibitors to specifically target and neutralize toxin A can reduce the likelihood of recurrence, offering a more sustainable long-term treatment strategy.
Moreover, TcdA inhibitors could have broader applications in managing other diseases influenced by similar bacterial toxins. For instance, other pathogenic bacteria produce toxins with mechanisms of action similar to TcdA. Understanding the effectiveness of TcdA inhibitors could pave the way for the development of inhibitors for these other toxins, broadening the scope of treatment options for various toxin-mediated diseases.
In conclusion, TcdA inhibitors represent a promising advancement in the treatment of Clostridioides difficile infections. By specifically targeting the toxin A molecule, these inhibitors offer a targeted approach that can mitigate the symptoms of CDI, reduce recurrence rates, and potentially offer new treatment avenues for other toxin-mediated diseases. As research continues to advance, the hope is that TcdA inhibitors will become an integral part of the therapeutic arsenal against C. difficile and other pathogenic bacteria.
How to obtain the latest development progress of all targets?
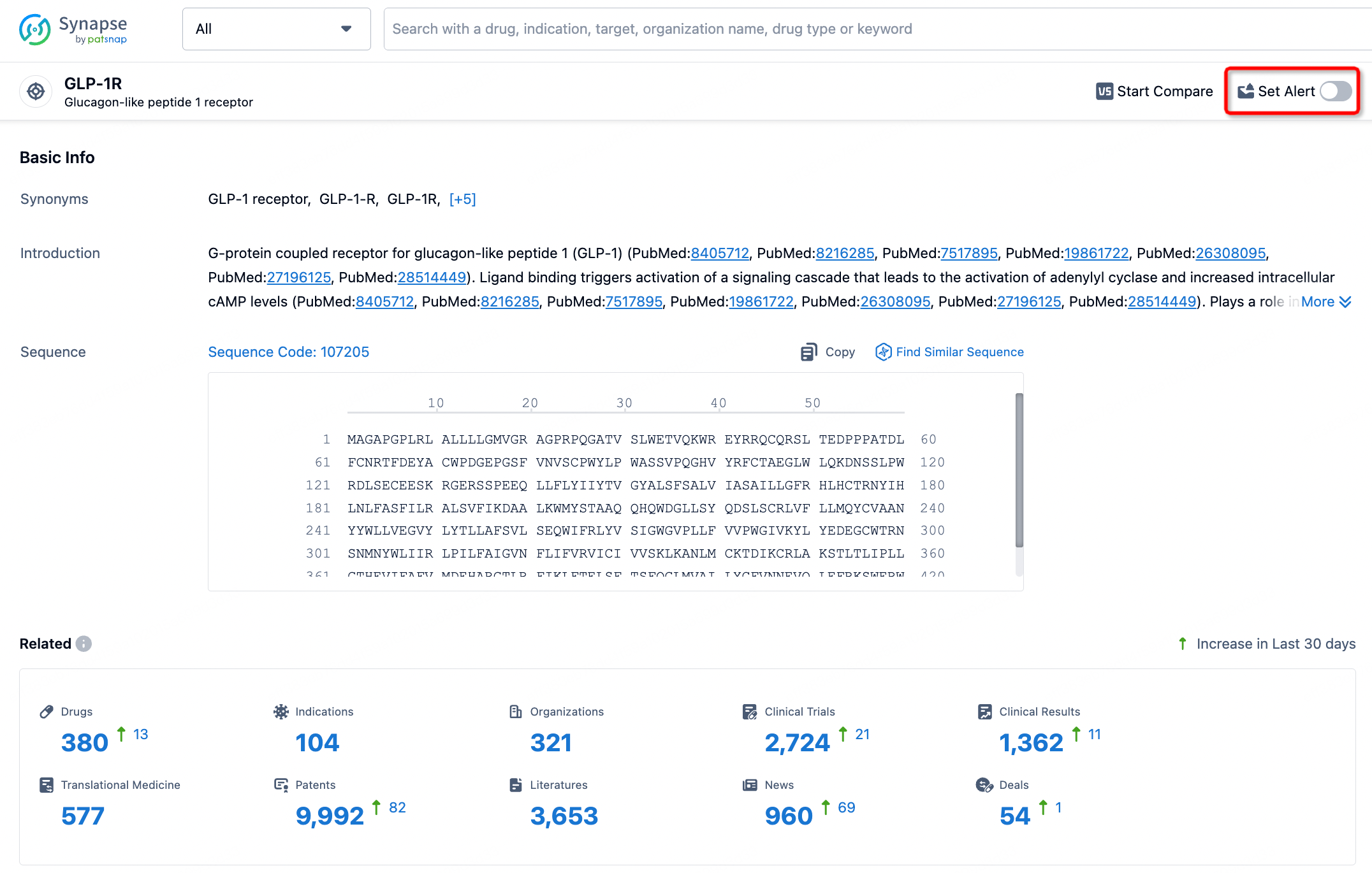
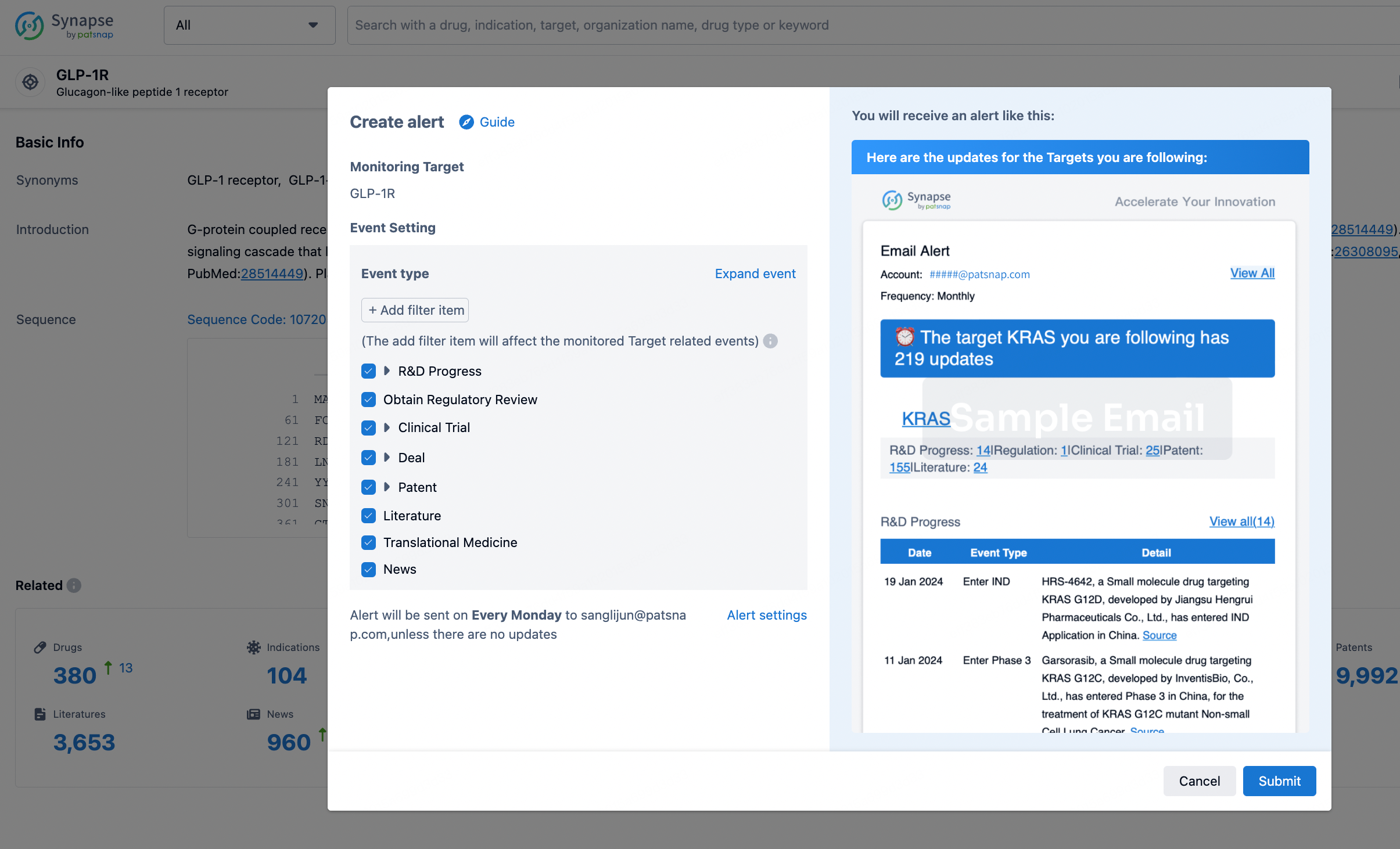
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.