Request Demo
What is Bortezomib used for?
14 June 2024
Bortezomib, known by its trade name as Velcade, is a proteasome inhibitor that represents a significant advancement in the treatment of certain types of cancer, particularly multiple myeloma and mantle cell lymphoma. Initially developed by Millennium Pharmaceuticals and later by Takeda Oncology, Bortezomib was first approved by the FDA in 2003. It marked a breakthrough in cancer therapies by targeting the ubiquitin-proteasome pathway, a system critical for protein degradation and regulation within cells. The drug has since been the subject of extensive research and clinical trials, expanding its indications and refining its application in oncology.
The mechanism of action of Bortezomib is primarily through the inhibition of the 26S proteasome, a complex enzyme responsible for degrading ubiquitinated proteins. By inhibiting this proteasome, Bortezomib disrupts the regulated degradation of proteins, leading to an accumulation of misfolded or damaged proteins within the cell. This accumulation triggers cellular stress responses, ultimately leading to apoptosis, or programmed cell death, particularly in malignant cells that rely on the proteasome for survival and proliferation. This selective toxicity is what makes Bortezomib an effective agent against cancer cells while sparing more normal cells.
Bortezomib is typically administered via injection, either intravenously (IV) or subcutaneously (under the skin). The choice of administration route may depend on various factors including patient tolerance and specific clinical circumstances. The standard regimen often involves a series of cycles, with the drug given on specific days followed by a rest period. This cyclical approach helps to maximize cancer cell kill while allowing normal cells time to recover. The onset of action is relatively rapid, with pharmacokinetic studies showing that Bortezomib reaches peak plasma concentration within 30 minutes to an hour after administration. However, the full therapeutic effects, such as tumor shrinkage or remission, may take several weeks or months to become evident, depending on the individual patient's response and the type of cancer being treated.
Despite its efficacy, Bortezomib is associated with a range of potential side effects that need to be carefully managed. Common adverse effects include fatigue, gastrointestinal disturbances (such as nausea, vomiting, and diarrhea), peripheral neuropathy (a painful condition affecting the nerves), and hematological issues like thrombocytopenia (low platelet count) and neutropenia (low white blood cell count). Peripheral neuropathy, in particular, can be dose-limiting and may necessitate a reduction in dosage or a change in the administration schedule. Other serious side effects can include heart problems, liver dysfunction, and rare cases of tumor lysis syndrome, a rapid release of cellular contents caused by the destruction of cancer cells that can lead to severe metabolic disturbances.
There are also several contraindications for Bortezomib use. It is generally contraindicated in patients with known hypersensitivity to Bortezomib, boron, or mannitol. Additionally, patients with severe hepatic impairment or those who are pregnant should not use Bortezomib due to potential risks to the liver and fetus, respectively. Careful consideration and adjustment of dosage may be required for patients with moderate hepatic impairment or those on dialysis for renal issues.
The pharmacokinetics and therapeutic efficacy of Bortezomib can be influenced by interactions with other drugs. For instance, drugs that are strong inhibitors or inducers of cytochrome P450 3A4 (CYP3A4) can affect Bortezomib metabolism. Co-administration with ketoconazole, a potent CYP3A4 inhibitor, can increase Bortezomib plasma levels, potentially enhancing its effects and side effects. Conversely, drugs that induce CYP3A4, such as rifampin, can reduce Bortezomib plasma levels, potentially decreasing its efficacy. Additionally, concomitant use with other chemotherapeutic agents or immunosuppressants that have overlapping toxicities, such as those causing bone marrow suppression or peripheral neuropathy, can exacerbate these adverse effects.
In summary, Bortezomib (Velcade) represents a cornerstone in the management of multiple myeloma and mantle cell lymphoma, offering a targeted approach through proteasome inhibition. Its administration is typically through IV or subcutaneous injection, with a well-established regimen designed to balance efficacy with tolerability. While it has transformed outcomes for many patients, the potential for significant side effects and drug interactions necessitates careful patient monitoring and may require adjustments in therapy. Ongoing research continues to explore ways to optimize its use, minimize its adverse effects, and expand its indications across a broader range of malignancies.
The mechanism of action of Bortezomib is primarily through the inhibition of the 26S proteasome, a complex enzyme responsible for degrading ubiquitinated proteins. By inhibiting this proteasome, Bortezomib disrupts the regulated degradation of proteins, leading to an accumulation of misfolded or damaged proteins within the cell. This accumulation triggers cellular stress responses, ultimately leading to apoptosis, or programmed cell death, particularly in malignant cells that rely on the proteasome for survival and proliferation. This selective toxicity is what makes Bortezomib an effective agent against cancer cells while sparing more normal cells.
Bortezomib is typically administered via injection, either intravenously (IV) or subcutaneously (under the skin). The choice of administration route may depend on various factors including patient tolerance and specific clinical circumstances. The standard regimen often involves a series of cycles, with the drug given on specific days followed by a rest period. This cyclical approach helps to maximize cancer cell kill while allowing normal cells time to recover. The onset of action is relatively rapid, with pharmacokinetic studies showing that Bortezomib reaches peak plasma concentration within 30 minutes to an hour after administration. However, the full therapeutic effects, such as tumor shrinkage or remission, may take several weeks or months to become evident, depending on the individual patient's response and the type of cancer being treated.
Despite its efficacy, Bortezomib is associated with a range of potential side effects that need to be carefully managed. Common adverse effects include fatigue, gastrointestinal disturbances (such as nausea, vomiting, and diarrhea), peripheral neuropathy (a painful condition affecting the nerves), and hematological issues like thrombocytopenia (low platelet count) and neutropenia (low white blood cell count). Peripheral neuropathy, in particular, can be dose-limiting and may necessitate a reduction in dosage or a change in the administration schedule. Other serious side effects can include heart problems, liver dysfunction, and rare cases of tumor lysis syndrome, a rapid release of cellular contents caused by the destruction of cancer cells that can lead to severe metabolic disturbances.
There are also several contraindications for Bortezomib use. It is generally contraindicated in patients with known hypersensitivity to Bortezomib, boron, or mannitol. Additionally, patients with severe hepatic impairment or those who are pregnant should not use Bortezomib due to potential risks to the liver and fetus, respectively. Careful consideration and adjustment of dosage may be required for patients with moderate hepatic impairment or those on dialysis for renal issues.
The pharmacokinetics and therapeutic efficacy of Bortezomib can be influenced by interactions with other drugs. For instance, drugs that are strong inhibitors or inducers of cytochrome P450 3A4 (CYP3A4) can affect Bortezomib metabolism. Co-administration with ketoconazole, a potent CYP3A4 inhibitor, can increase Bortezomib plasma levels, potentially enhancing its effects and side effects. Conversely, drugs that induce CYP3A4, such as rifampin, can reduce Bortezomib plasma levels, potentially decreasing its efficacy. Additionally, concomitant use with other chemotherapeutic agents or immunosuppressants that have overlapping toxicities, such as those causing bone marrow suppression or peripheral neuropathy, can exacerbate these adverse effects.
In summary, Bortezomib (Velcade) represents a cornerstone in the management of multiple myeloma and mantle cell lymphoma, offering a targeted approach through proteasome inhibition. Its administration is typically through IV or subcutaneous injection, with a well-established regimen designed to balance efficacy with tolerability. While it has transformed outcomes for many patients, the potential for significant side effects and drug interactions necessitates careful patient monitoring and may require adjustments in therapy. Ongoing research continues to explore ways to optimize its use, minimize its adverse effects, and expand its indications across a broader range of malignancies.
How to obtain the latest development progress of all drugs?
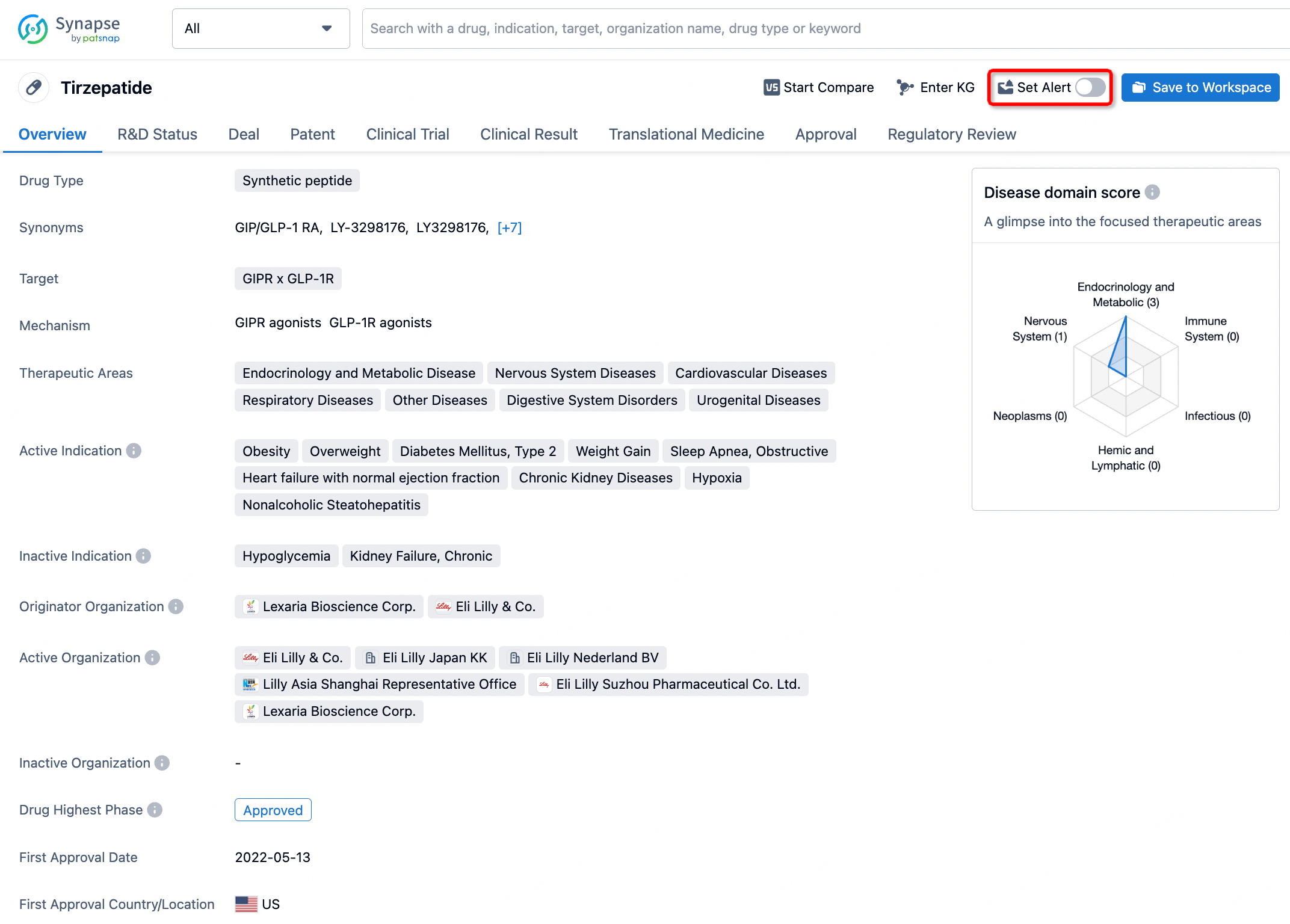
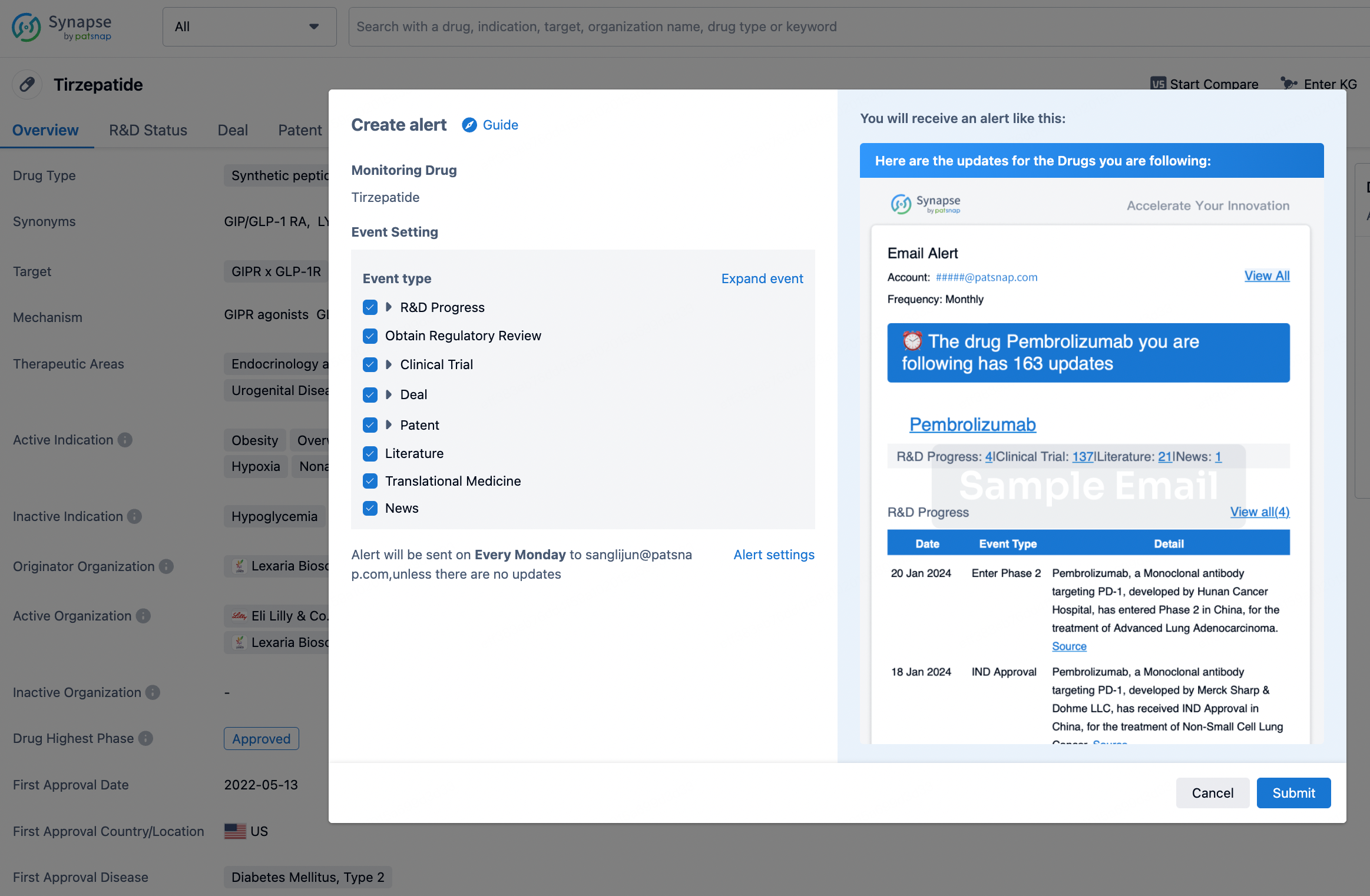
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.