Request Demo
What is the mechanism of Ibrutinib?
17 July 2024
Ibrutinib, a breakthrough medication in the treatment of various B-cell malignancies, has garnered significant attention for its effectiveness and unique mechanism of action. It is primarily used to treat conditions such as chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström's macroglobulinemia (WM). To understand how ibrutinib works, it's important to delve into the specifics of its mechanism at the molecular level.
Ibrutinib is an inhibitor of Bruton's tyrosine kinase (BTK), an enzyme crucial for the signaling pathways that drive the growth and survival of B-cells. BTK is a part of the B-cell receptor (BCR) signaling pathway. In normal physiology, BCR signaling helps in the development and function of B-cells, which produce antibodies as part of the immune response. However, in certain B-cell malignancies, this signaling pathway is dysregulated, leading to uncontrolled proliferation and survival of malignant B-cells.
BTK plays a pivotal role in transmitting signals from the BCR to the nucleus of the cell, promoting the activation of genes that lead to cell growth and survival. By inhibiting BTK, ibrutinib effectively disrupts this signaling cascade. Specifically, ibrutinib covalently binds to the cysteine residue C481 in the active site of BTK. This irreversible binding inhibits the kinase activity of BTK, thereby blocking downstream signaling pathways that include the activation of proteins such as PLCγ2, AKT, and NF-κB, which are essential for B-cell survival and proliferation.
The inhibition of BTK by ibrutinib leads to several downstream effects, including reduced proliferation of malignant B-cells, increased apoptosis (programmed cell death), and impaired homing and adhesion of B-cells. By preventing malignant B-cells from receiving survival signals, ibrutinib effectively reduces the number of these cancerous cells in the body.
In addition to its direct effects on BCR signaling, ibrutinib also impacts other signaling pathways and interactions within the tumor microenvironment. For example, it inhibits the chemokine receptors CXCR4 and CXCR5, which play roles in the migration and localization of B-cells within lymphoid tissues. By disrupting these pathways, ibrutinib further hampers the ability of malignant B-cells to thrive and spread.
Clinical studies have demonstrated that ibrutinib is highly effective in inducing remissions and prolonging survival in patients with CLL, MCL, and WM. Its success has led to its approval by regulatory agencies and its widespread adoption in clinical practice. However, like all medications, ibrutinib is not without side effects. Common adverse effects include diarrhea, fatigue, musculoskeletal pain, and an increased risk of bleeding and infections. Careful monitoring and management of these side effects are essential to ensure optimal outcomes for patients.
In summary, ibrutinib's mechanism of action fundamentally revolves around its ability to inhibit BTK, thereby disrupting critical signaling pathways necessary for the survival and proliferation of malignant B-cells. This targeted approach has proven to be a powerful strategy in treating B-cell malignancies and continues to be a focal point of ongoing research and development in the field of oncology.
Ibrutinib is an inhibitor of Bruton's tyrosine kinase (BTK), an enzyme crucial for the signaling pathways that drive the growth and survival of B-cells. BTK is a part of the B-cell receptor (BCR) signaling pathway. In normal physiology, BCR signaling helps in the development and function of B-cells, which produce antibodies as part of the immune response. However, in certain B-cell malignancies, this signaling pathway is dysregulated, leading to uncontrolled proliferation and survival of malignant B-cells.
BTK plays a pivotal role in transmitting signals from the BCR to the nucleus of the cell, promoting the activation of genes that lead to cell growth and survival. By inhibiting BTK, ibrutinib effectively disrupts this signaling cascade. Specifically, ibrutinib covalently binds to the cysteine residue C481 in the active site of BTK. This irreversible binding inhibits the kinase activity of BTK, thereby blocking downstream signaling pathways that include the activation of proteins such as PLCγ2, AKT, and NF-κB, which are essential for B-cell survival and proliferation.
The inhibition of BTK by ibrutinib leads to several downstream effects, including reduced proliferation of malignant B-cells, increased apoptosis (programmed cell death), and impaired homing and adhesion of B-cells. By preventing malignant B-cells from receiving survival signals, ibrutinib effectively reduces the number of these cancerous cells in the body.
In addition to its direct effects on BCR signaling, ibrutinib also impacts other signaling pathways and interactions within the tumor microenvironment. For example, it inhibits the chemokine receptors CXCR4 and CXCR5, which play roles in the migration and localization of B-cells within lymphoid tissues. By disrupting these pathways, ibrutinib further hampers the ability of malignant B-cells to thrive and spread.
Clinical studies have demonstrated that ibrutinib is highly effective in inducing remissions and prolonging survival in patients with CLL, MCL, and WM. Its success has led to its approval by regulatory agencies and its widespread adoption in clinical practice. However, like all medications, ibrutinib is not without side effects. Common adverse effects include diarrhea, fatigue, musculoskeletal pain, and an increased risk of bleeding and infections. Careful monitoring and management of these side effects are essential to ensure optimal outcomes for patients.
In summary, ibrutinib's mechanism of action fundamentally revolves around its ability to inhibit BTK, thereby disrupting critical signaling pathways necessary for the survival and proliferation of malignant B-cells. This targeted approach has proven to be a powerful strategy in treating B-cell malignancies and continues to be a focal point of ongoing research and development in the field of oncology.
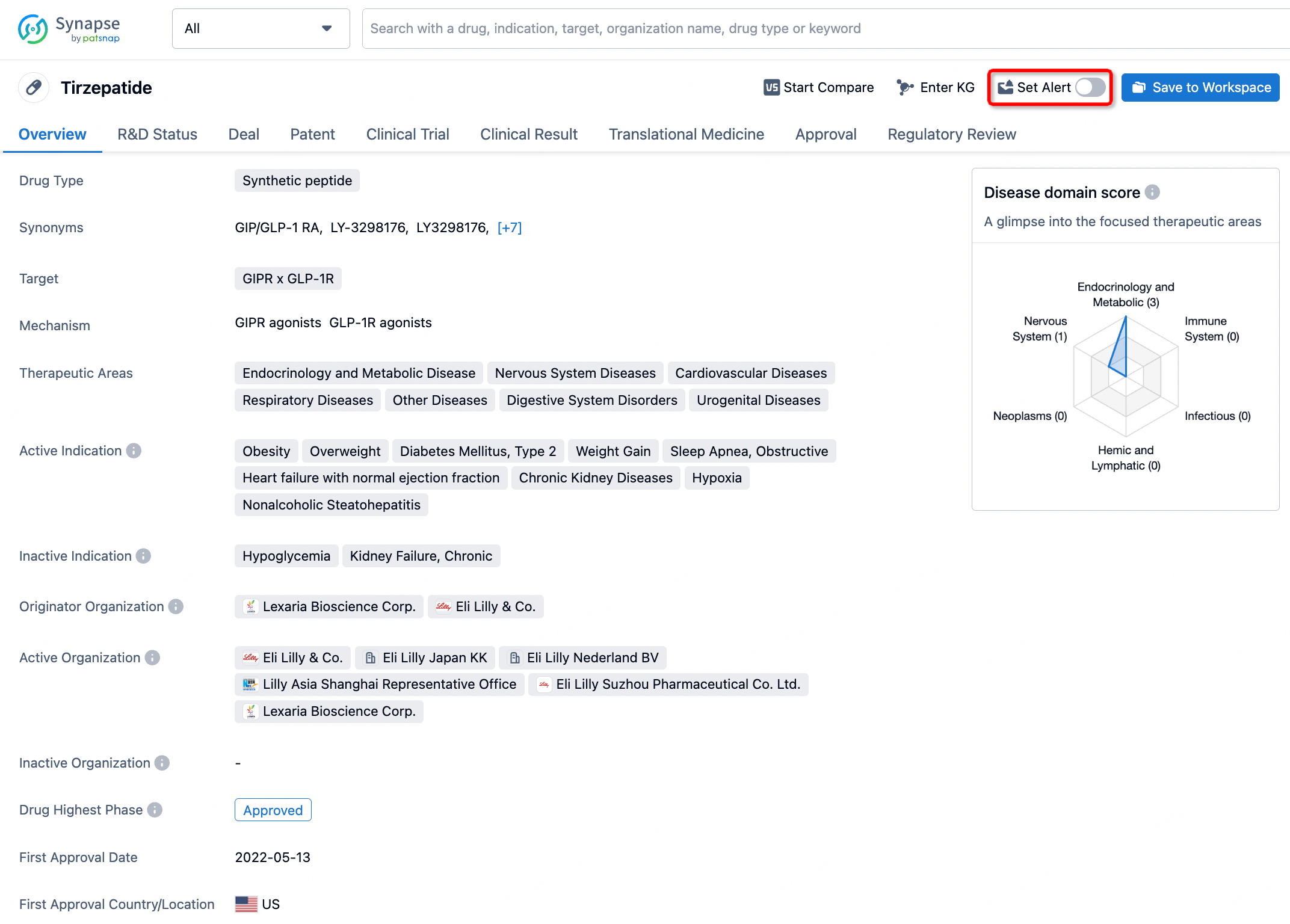
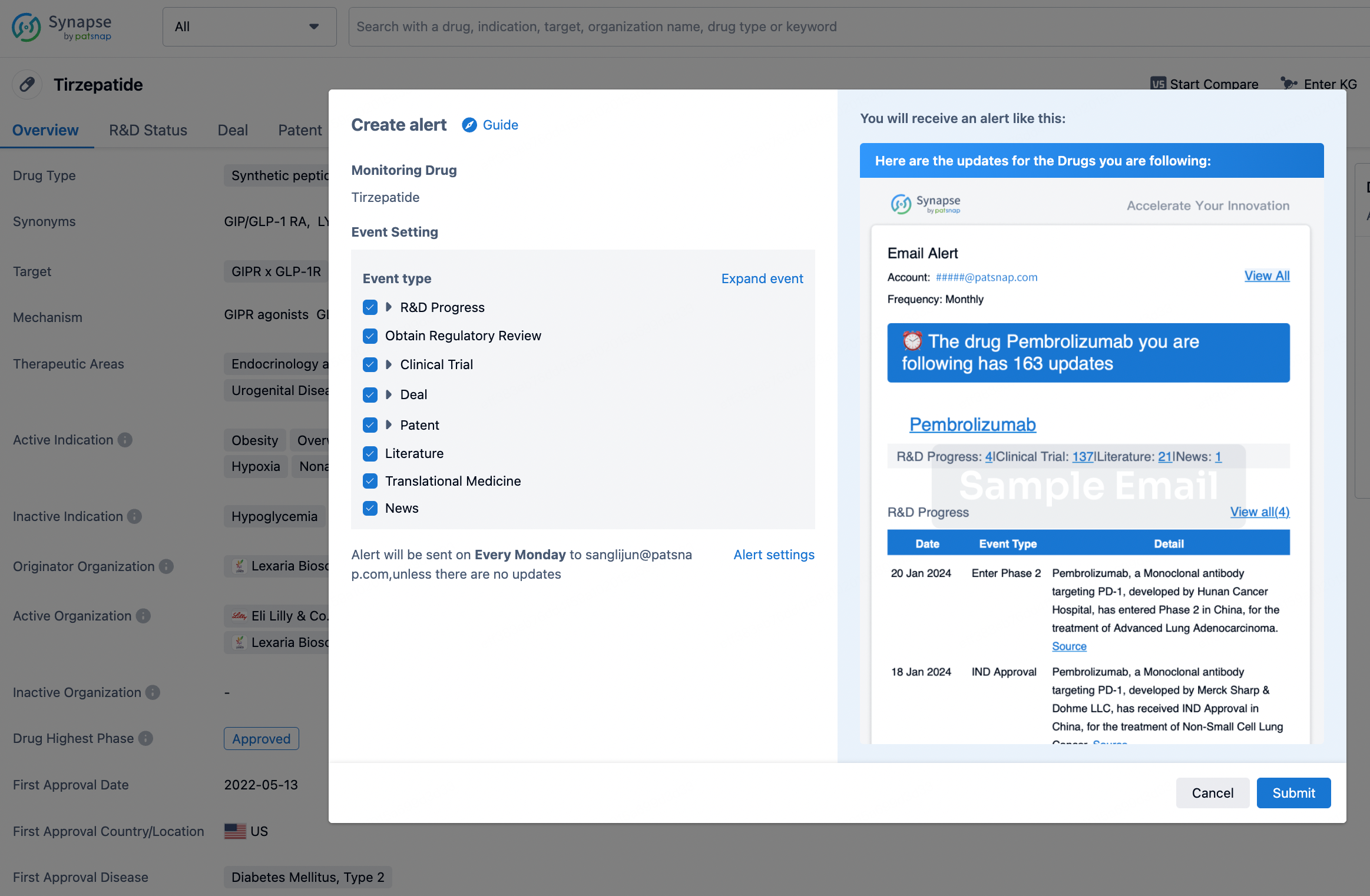
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.