Request Demo
What is the mechanism of Mepivacaine Hydrochloride?
18 July 2024
Mepivacaine Hydrochloride is a widely used local anesthetic, particularly in dental and minor surgical procedures. Understanding its mechanism of action provides insights into how it effectively blocks pain and sensory perception in targeted areas.
Mepivacaine Hydrochloride belongs to the amide class of local anesthetics, which are known for their stability and low incidence of allergic reactions compared to ester-based anesthetics. Its mechanism primarily involves the blockade of sodium channels in neuronal cell membranes, which is crucial for the propagation of nerve impulses.
When mepivacaine is administered, it diffuses through the neuronal membrane in its uncharged, lipophilic form. Once inside the neuron, it becomes protonated in the slightly acidic intracellular environment. This ionized form is capable of binding to the intracellular portion of voltage-gated sodium channels. Normally, these channels allow sodium ions to enter the neuron, leading to depolarization and the generation of an action potential. By blocking these channels, mepivacaine prevents the influx of sodium ions, thereby inhibiting the initiation and transmission of nerve impulses. As a result, the sensation of pain is temporarily lost in the area of administration.
In addition to its primary action on sodium channels, mepivacaine may also exert minor effects on potassium and calcium channels, although these are not as well characterized. Furthermore, its interaction with various receptor sites and interference with the release of neurotransmitters can contribute to its overall anesthetic effect.
The onset and duration of mepivacaine's action depend on several factors including the specific formulation used, the site of administration, and the presence of vasoconstrictors like epinephrine. Typically, mepivacaine has a rapid onset of action, often within minutes, and provides anesthesia for approximately 2 to 3 hours. The addition of a vasoconstrictor can prolong its effects by reducing local blood flow, thereby slowing the systemic absorption of the drug.
Mepivacaine is metabolized primarily in the liver by cytochrome P450 enzymes, specifically CYP1A2 and CYP3A4, and is subsequently excreted in the urine. Its metabolic byproducts are generally less active than the parent compound and are eliminated from the body within a few hours. However, factors such as liver function, age, and concurrent medications can influence the metabolism and clearance of mepivacaine, necessitating dose adjustments in certain populations.
Clinically, mepivacaine is chosen for its intermediate duration of action and lower incidence of vasodilation compared to other local anesthetics like lidocaine. This makes it particularly useful in patients where excessive bleeding or prolonged numbness is a concern. Additionally, its lower systemic toxicity profile allows for safer administration in larger volumes when necessary.
In conclusion, the mechanism of action of mepivacaine hydrochloride involves the blockade of voltage-gated sodium channels in neuronal membranes, preventing the propagation of nerve impulses and thereby achieving localized anesthesia. Its pharmacokinetic properties, rapid onset, and intermediate duration make it a versatile and effective option for various medical and dental procedures. Understanding these mechanisms can help healthcare providers optimize its use for maximum efficacy and safety.
Mepivacaine Hydrochloride belongs to the amide class of local anesthetics, which are known for their stability and low incidence of allergic reactions compared to ester-based anesthetics. Its mechanism primarily involves the blockade of sodium channels in neuronal cell membranes, which is crucial for the propagation of nerve impulses.
When mepivacaine is administered, it diffuses through the neuronal membrane in its uncharged, lipophilic form. Once inside the neuron, it becomes protonated in the slightly acidic intracellular environment. This ionized form is capable of binding to the intracellular portion of voltage-gated sodium channels. Normally, these channels allow sodium ions to enter the neuron, leading to depolarization and the generation of an action potential. By blocking these channels, mepivacaine prevents the influx of sodium ions, thereby inhibiting the initiation and transmission of nerve impulses. As a result, the sensation of pain is temporarily lost in the area of administration.
In addition to its primary action on sodium channels, mepivacaine may also exert minor effects on potassium and calcium channels, although these are not as well characterized. Furthermore, its interaction with various receptor sites and interference with the release of neurotransmitters can contribute to its overall anesthetic effect.
The onset and duration of mepivacaine's action depend on several factors including the specific formulation used, the site of administration, and the presence of vasoconstrictors like epinephrine. Typically, mepivacaine has a rapid onset of action, often within minutes, and provides anesthesia for approximately 2 to 3 hours. The addition of a vasoconstrictor can prolong its effects by reducing local blood flow, thereby slowing the systemic absorption of the drug.
Mepivacaine is metabolized primarily in the liver by cytochrome P450 enzymes, specifically CYP1A2 and CYP3A4, and is subsequently excreted in the urine. Its metabolic byproducts are generally less active than the parent compound and are eliminated from the body within a few hours. However, factors such as liver function, age, and concurrent medications can influence the metabolism and clearance of mepivacaine, necessitating dose adjustments in certain populations.
Clinically, mepivacaine is chosen for its intermediate duration of action and lower incidence of vasodilation compared to other local anesthetics like lidocaine. This makes it particularly useful in patients where excessive bleeding or prolonged numbness is a concern. Additionally, its lower systemic toxicity profile allows for safer administration in larger volumes when necessary.
In conclusion, the mechanism of action of mepivacaine hydrochloride involves the blockade of voltage-gated sodium channels in neuronal membranes, preventing the propagation of nerve impulses and thereby achieving localized anesthesia. Its pharmacokinetic properties, rapid onset, and intermediate duration make it a versatile and effective option for various medical and dental procedures. Understanding these mechanisms can help healthcare providers optimize its use for maximum efficacy and safety.
How to obtain the latest development progress of all drugs?
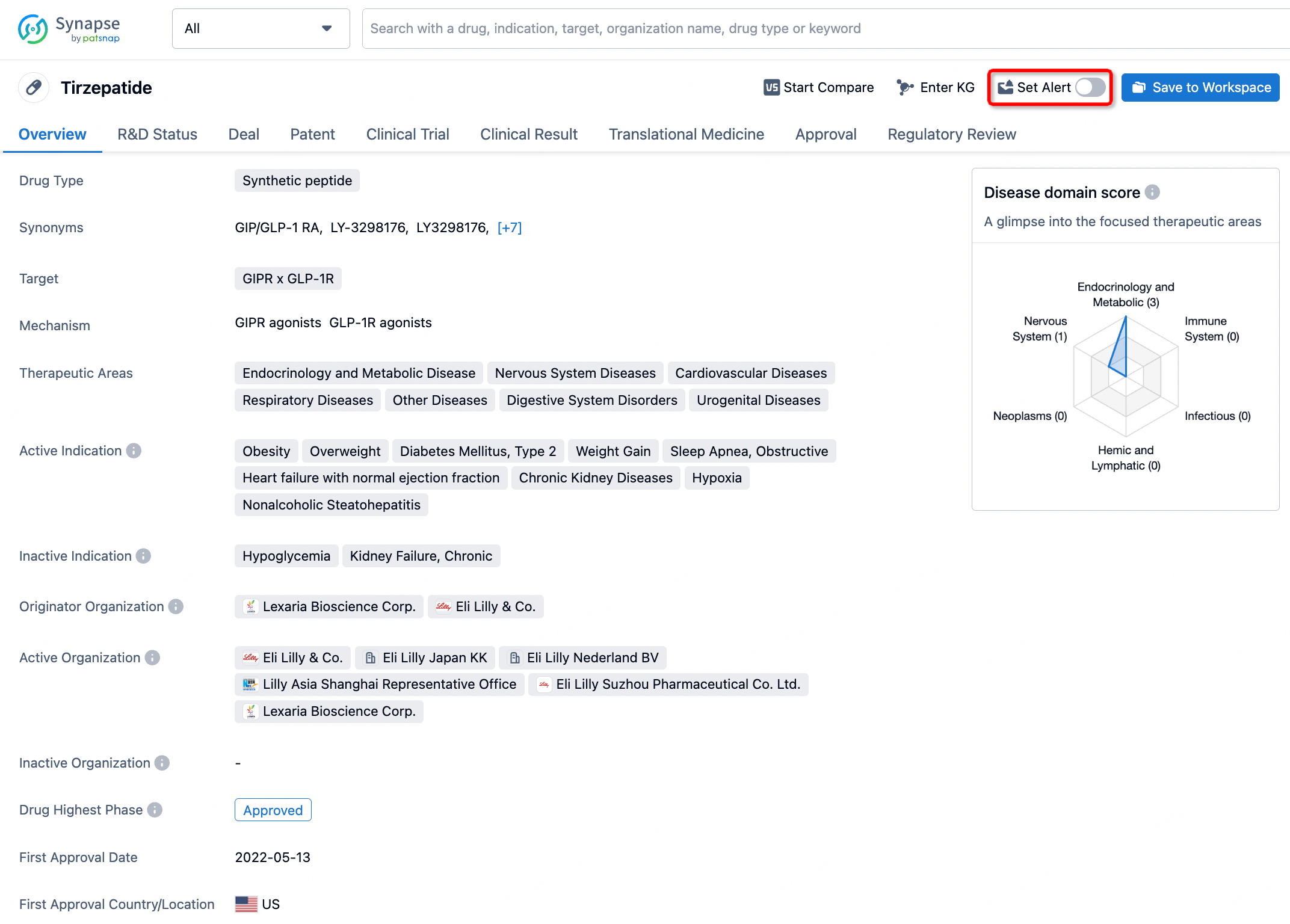
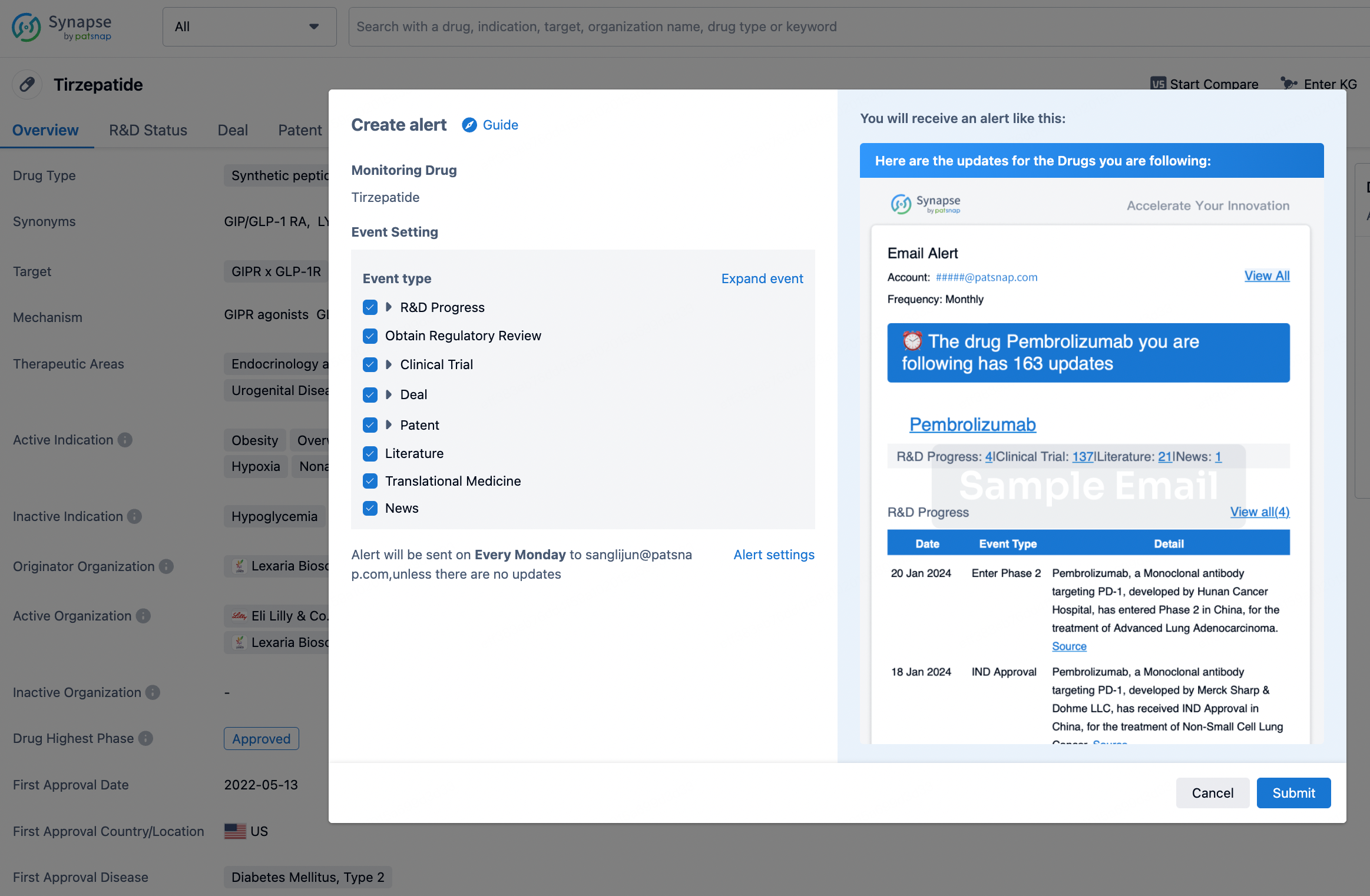
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.