Analysis on the Research Progress of Endothelin Receptor Antagonist
Endothelin receptor are G protein-coupled receptors (GPCRs) of the β-group of rhodopsin receptors that bind to endothelin ligands, which are 21 amino acid long peptides derived from longer prepro-endothelin precursors. There are at least four types known, ETA, ETB (ETB1, ETB2) and ETC. The ETA receptor is characterized by having high affinity and selectivity for ET-1 and ET-2 compared to ET-3, whereas the ETB receptor has equivalent high affinity for all three endothelin isopeptides.
Endothelin is a small molecule primarily secreted by vascular endothelium, with its receptors predominantly expressed in endothelial cells and vascular smooth muscle cells. Endothelin is related to cell proliferation and pulmonary vascular contraction. Research has reported that the concentration of endothelin in the serum of PAH patients is significantly increased, and the expression of endothelin receptors in vascular smooth muscle cells is overexpressed. The targets of endothelin receptor antagonists are endothelin receptors A and B.
Endothelin (ET) is divided into ET-1, ET-2, and ET-3. ET-1 is currently known as the most potent vasoconstrictor of vascular smooth muscle, and it is involved in maintaining normal blood pressure and promoting the proliferation of smooth muscle cells and endothelial cells. For endothelin A receptors, the affinity order of ET is ET-1 > ET-2 > ET-3; for endothelin B receptors, the affinity of the three ETs is equal. The A receptor is predominantly expressed in smooth muscle cells, and the B receptor is more abundant in endothelial cells. The vasoconstriction function of ET-1 is regulated by the A receptor, and the B receptor relaxes blood vessels by releasing nitric oxide.
Endothelins are synthesized in several tissues, including the vascular endothelium (ET-1 exclusively) and smooth muscle cells. Released endothelin binds to the endothelin receptors ETA and ETB, the ETA receptors on vascular smooth muscle cells mediating vasoconstriction, and the ETB receptors on the endothelium linked to nitric oxide (NO) and prostacyclin release.
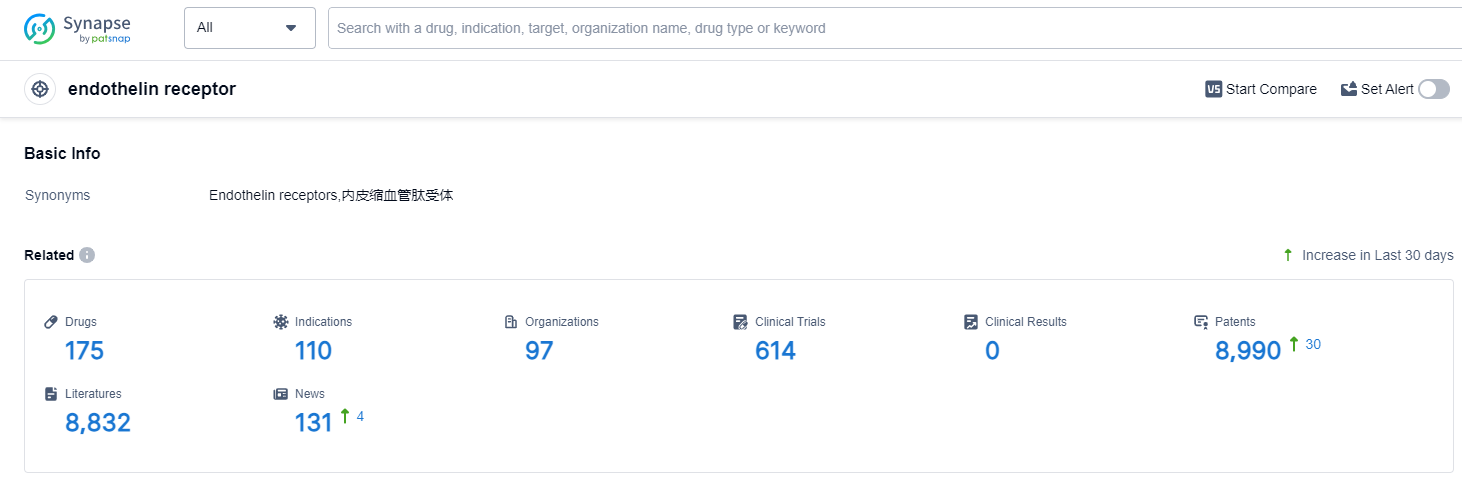
Endothelin receptor Competitive Landscape
According to Patsnap Synapse, as of 13 Oct 2023, there are a total of 175 endothelin receptor drugs worldwide, from 97 organizations, covering 110 indications, and conducting 614 clinical trials..
👇Please click on the picture link below for free registration or login directly if you have freemium accounts, you can browse the latest research progress on drugs , indications, organizations, clinical trials, clinical results, and drug patents related to this target.
The current competitive landscape of the target endothelin receptor is characterized by the presence of multiple companies with drugs in various stages of development. Johnson & Johnson, GSK Plc, Idorsia Ltd., Pharmazz, Inc., and Gilead Sciences, Inc. are some of the companies with significant R&D progress in this area. The Approved phase has the highest number of drugs, indicating successful development and regulatory approval for specific indications such as Pulmonary Arterial Hypertension, Glomerulonephritis, IGA, and Subarachnoid Hemorrhage.
Small molecule drugs and Synthetic peptides are the most rapidly progressing drug types, suggesting potential competition around innovative drugs. Further analysis is required to determine the research and development institutions of these biosimilars.
The United States, Japan, and European Union are leading in terms of drug development under the target endothelin receptor. China has also made progress, although the number of drugs in development is relatively small compared to other countries.
Overall, the target endothelin receptor presents opportunities for further research and development, with potential for innovative drugs to address various indications and meet unmet medical needs
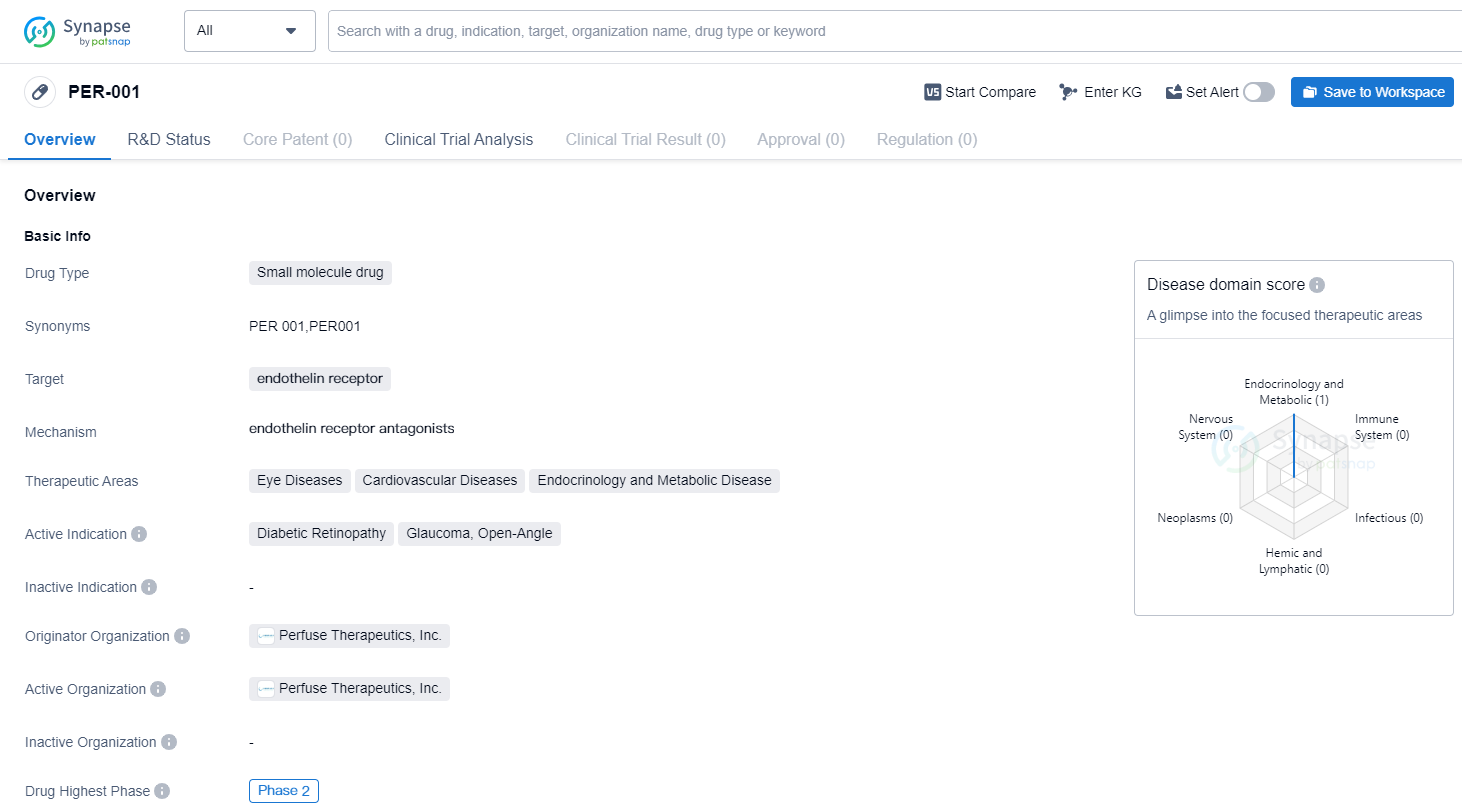
Vitreous Implant - PER-001 for the Treatment of Diabetic Retinopathy
PER-001 is a small molecule drug that targets the endothelin receptor. It is being developed by Perfuse Therapeutics, Inc., a pharmaceutical company specializing in biomedicine. The drug is currently in Phase 2, which is the highest phase of clinical development globally.
PER-001 has shown potential therapeutic benefits in various therapeutic areas, including eye diseases, cardiovascular diseases, and endocrinology and metabolic diseases. Specifically, it has demonstrated efficacy in treating diabetic retinopathy, glaucoma (open-angle), and other related eye conditions.
👇Please click on the image below to directly access the latest data (R&D Status | Core Patent | Clinical Trial | Approval status in Global countries) of this drug.
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina, leading to vision impairment or even blindness. Glaucoma, on the other hand, is a group of eye conditions that damage the optic nerve, often caused by increased pressure in the eye. Open-angle glaucoma is the most common form of glaucoma, characterized by a gradual loss of peripheral vision.
The targeting of the endothelin receptor by PER-001 suggests that it may have a mechanism of action related to regulating blood vessel constriction and inflammation. This could potentially be beneficial in treating the aforementioned eye diseases, as well as cardiovascular diseases and endocrinology and metabolic diseases. However, further research and clinical trials are needed to fully understand the drug's efficacy and safety profile.
As PER-001 is currently in Phase 2, it indicates that the drug has already undergone initial safety testing and has shown promising results in early-stage clinical trials. Phase 2 trials typically involve a larger number of participants and aim to further evaluate the drug's effectiveness and side effects. If the drug continues to show positive results in Phase 2, it may progress to Phase 3 trials, which involve an even larger patient population and are crucial for obtaining regulatory approval.
In summary, PER-001 is a small molecule drug developed by Perfuse Therapeutics, Inc. that targets the endothelin receptor. It has shown potential in treating various eye diseases, including diabetic retinopathy and glaucoma (open-angle), as well as cardiovascular diseases and endocrinology and metabolic diseases. With its current status in Phase 2, further research and clinical trials will determine its potential as a therapeutic option in these therapeutic areas.
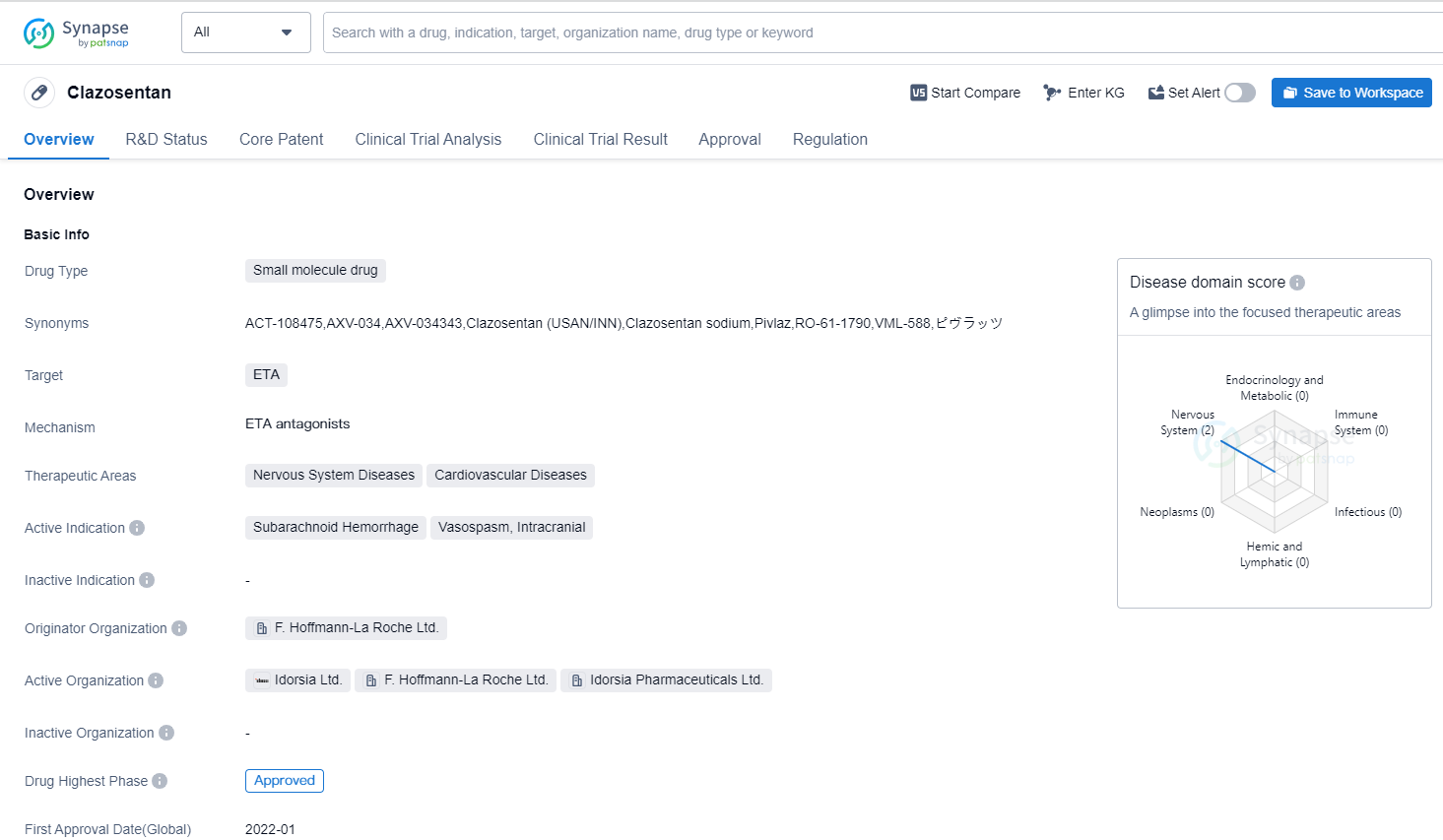
Clazosentan——Hope for Preventing Vasospasm after Subarachnoid Hemorrhage (SAH)
Clazosentan is a small molecule drug that falls under the therapeutic areas of Nervous System Diseases and Cardiovascular Diseases. It specifically targets the ETA receptor. The drug is primarily indicated for the treatment of Subarachnoid Hemorrhage, Vasospasm, and Intracranial conditions.
Clazosentan was developed by F. Hoffmann-La Roche Ltd., a renowned pharmaceutical organization. As of the latest available information, the drug has reached the highest phase of approval globally. However, its highest phase in China is still pending.
👇Please click on the image below to directly access the latest data (R&D Status | Core Patent | Clinical Trial | Approval status in Global countries) of this drug.
The global first approval of Clazosentan took place in January 2022, with Japan being the country/location where it was first approved. It is important to note that Clazosentan is regulated as an orphan drug. Orphan drugs are medications developed to treat rare diseases or conditions that affect a small number of patients.
Aneurysmal subarachnoid hemorrhage (aSAH) is a sudden, life-threatening condition caused by the rupture of an aneurysm. It necessitates emergency surgery, including endovascular coiling or surgical microclipping, to prevent re-rupture. The dissolution of blood clots and the release of vasoconstrictive substances can induce cerebral vasospasm, typically commencing about 3 days after an aSAH attack, peaking on days 8-11, and subsiding on day 21.3. If left untreated, cerebral vasospasm may be a key factor in morbidity and mortality in patients with aSAH. Delayed ischemic neurological deficits (DIND), resulting from cerebral vasospasm, account for 17-40% of aSAH, and half of the patients with vasospasm develop cerebral infarction.
Nimodipine, a calcium channel blocker (administered orally or via intravenous injection), has become the standard treatment in the US and Europe for improving neurological prognosis following subarachnoid hemorrhage, but there is no convincing evidence that it affects the incidence of vasospasm or DIND. In Japan, intravenous fasudil hydrochloride (a Rho-kinase inhibitor) and intravenous ozagrel sodium (a thromboxane A2 synthase inhibitor) have been used to prevent vasospasm. However, the number of studies on these drugs is limited, and their impact on DIND and outcomes remains uncertain.
Endothelin-1 (ET-1) has potent and persistent vasoconstrictive effects. A large amount of ET-1 is produced after aSAH, making it a key factor in the development of cerebral vasospasm. Clazosentan is an endothelin receptor antagonist (ERA) that has been extensively studied for the prevention of cerebral vasospasm in patients with aSAH.
The CONSCIOUS-1 study demonstrated that Clazosentan reduces the incidence of moderate to severe vasospasm in patients with aSAH who have undergone aneurysm clamping or occlusion. This effect is dose-dependent, with a relative risk reduction (RRR) of up to 65%. Subsequent CONSCIOUS-2 and CONSCIOUS-3 trials investigated the impact of Clazosentan on the morbidity and all-cause mortality associated with cerebral vasospasm. CONSCIOUS-2 showed that Clazosentan at a dose of 5 mg/hour did not yield statistically significant treatment results, leading to the early termination of the CONSCIOUS-3 trial. However, an exploratory analysis of CONSCIOUS-3 indicated that the RRR of morbidity and all-cause mortality associated with cerebral vasospasm at a dose of 15 mg/hr Clazosentan was 44%. Meanwhile, a phase II exploratory dose study conducted in Japan and South Korea found that 10 mg/hr of Clazosentan, compared to placebo, reduced the morbidity and all-cause mortality associated with cerebral vasospasm in patients with aSAH who underwent surgical clamping. Its tolerability was also similar to that of 5 mg/hr.
In December 2022, Teiji Tominaga and colleagues from Japan published their research findings in J Neurosurg, assessing the impact of Clazosentan on the incidence of cerebral vasospasm-related morbidity and all-cause mortality in Japanese patients with aneurysmal subarachnoid hemorrhage (aSAH).
This involved two similar double-blind, placebo-controlled phase III trials involving aSAH patients, accomplished by 57 Japanese centers. One trial enrolled aSAH patients with intravascular coil embolization of aneurysms, while another included aSAH patients who had undergone surgical clipping of aneurysms. In each study, Clazosentan (10mg/hr) or placebo (1:1) was randomly administered intravenously within 48 hours of SAH onset and continued until day 15. Stratification was based on the WFNS grading. The primary endpoints of each trial were the incidence of cerebral vasospasm-related morbidity and all-cause mortality within 6 weeks of aSAH, including new-onset cerebral infarction, delayed ischemic neurological deficit, and all-cause mortality.
In summary, Clazosentan is a small molecule drug developed by F. Hoffmann-La Roche Ltd. It targets the ETA receptor and is indicated for the treatment of Subarachnoid Hemorrhage, Vasospasm, and Intracranial conditions. The drug has reached the highest phase of approval globally and is regulated as an orphan drug. Its first approval occurred in Japan in January 2022. However, its highest phase in China is still pending.