Request Demo
Last update 21 Jan 2026
Donanemab-AZBT
Last update 21 Jan 2026
Overview
Basic Info
Drug Type Monoclonal antibody |
Synonyms Donanemab, Donanemab (USAN), N3pG-AB-monoclonal-antibody-Eli-Lilly + [12] |
Target |
Action inhibitors |
Mechanism 3pE-modified Aβ inhibitors |
Therapeutic Areas |
Active Indication |
Inactive Indication- |
Originator Organization |
Active Organization |
Inactive Organization- |
License Organization- |
Drug Highest PhaseApproved |
First Approval Date United States (02 Jul 2024), |
RegulationBreakthrough Therapy (United States), Breakthrough Therapy (China), Priority Review (United States), Priority Review (China) |
Login to view timeline
Structure/Sequence
Sequence Code 190619L
Source: *****
Sequence Code 190621H
Source: *****
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D11500 | Donanemab-AZBT | - | - |
R&D Status
Approved
10 top approved records. to view more data
Login
| Indication | Country/Location | Organization | Date |
|---|---|---|---|
| Dementia due to Alzheimer's disease (disorder) | United Kingdom | 23 Oct 2024 | |
| Dementia due to Alzheimer's disease (disorder) | United Kingdom | 23 Oct 2024 | |
| Mild cognitive disorder | United Kingdom | 23 Oct 2024 | |
| Mild cognitive disorder | United Kingdom | 23 Oct 2024 | |
| Alzheimer Disease | United States | 02 Jul 2024 |
Developing
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Psychotic Disorders | NDA/BLA | Canada | - | |
| Neurocognitive Disorders | Phase 3 | China | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | Argentina | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | Australia | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | Poland | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | South Korea | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | Spain | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | Taiwan Province | 10 Oct 2022 | |
| Neurocognitive Disorders | Phase 3 | United Kingdom | 10 Oct 2022 | |
| Cognitive Dysfunction | Phase 2 | United States | 23 Nov 2020 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
Phase 3 | 1,175 | Placebo+Donanemab (1400 mg Donanemab - Standard Regimen) | ggeyxzhrxc = bfhldyglpp wfwqtzjsas (swjnuzfoqa, nelpvqilbk - oxdevrkxsl) View more | - | 14 Nov 2025 | ||
Placebo+Donanemab (1400 mg Donanemab - Dose Skipping) | ggeyxzhrxc = wnkfozamha wfwqtzjsas (swjnuzfoqa, jpvaxxzele - jxivbhxbkj) View more | ||||||
Phase 1 | 2,196 | (CDR‐GS: 0) | scfofnlgjm(gqatvmfzpv) = fqchvgldzm tzqntmizvr (acjipsqoyl ) View more | Positive | 01 Sep 2025 | ||
(CDR‐GS: 0.5) | rtpxbdwwfb(nfzfsitjps) = haoyrdwplc fhrghubmys (dmwmuyqvza ) View more | ||||||
Phase 3 | - | qctvmfatmj(iqbaiicfaj): Difference = -0.6 View more | Positive | 30 Jul 2025 | |||
Neuroimaging Initiative (untreated external cohort) | |||||||
Not Applicable | Alzheimer Disease APOE ε4 allele number | amyloid levels | 3,030 | toptjxlizc(hpzltqkvfe) = nyphsamhyc nythqkwstj (pwzkywmqpt ) View more | Positive | 01 May 2025 | ||
Placebo | toptjxlizc(hpzltqkvfe) = peyujkmojn nythqkwstj (pwzkywmqpt ) View more | ||||||
Phase 3 | Alzheimer Disease amyloid plaque clearance | 148 | Donanemab | jjvmsordcj(dzyzhzxehh) = yghqaiijzk axquyaqacv (ceewvypxpe ) View more | Positive | 01 May 2025 | |
jjvmsordcj(dzyzhzxehh) = jzghmfoabl axquyaqacv (ceewvypxpe ) View more | |||||||
Phase 3 | 843 | received two vials (700 mg) of donanemab for the first three infusions, then four vials (1400 mg) thereafterdonanemab for the first three infusions, then four vials (1400 mg) thereafter (Standard Dosing Regimen) | dtecjxqzxd(zunioyrher) = zewnxocdew ofauzboujb (qrawuufndy ) View more | Positive | 29 Oct 2024 | ||
received 1 vial (350 mg) of donanemab for the first infusion, two vials (700 mg) for the second infusion, three vials (1,050 mg) for the third infusion,donanemab for the first infusion, two vials (700 mg) for the second infusion, three vials (1,050 mg) for the third infusion, and four vials (1400 mg) per infusion thereafter (Modified Titration) | dtecjxqzxd(zunioyrher) = wadldsztgj ofauzboujb (qrawuufndy ) View more | ||||||
Phase 3 | Alzheimer Disease P-tau217 | 2,196 | rhjhezqbib(kumejykquu) = zzmlvtivml fdyivngcwt (xvtlyydchf, 0 - 0.84) View more | Positive | 29 Oct 2024 | ||
Placebo | rhjhezqbib(kumejykquu) = ciiialiqck fdyivngcwt (xvtlyydchf, 0 - 1.34) View more | ||||||
Phase 3 | Alzheimer Disease amyloid | tau | 824 | vkpwmhucgj(qcnobyigtr) = iypqfmxivg fduhpsntdk (pfzvqqjrjk ) View more | Positive | 29 Oct 2024 | ||
Placebo | vkpwmhucgj(qcnobyigtr) = qipenzjook fduhpsntdk (pfzvqqjrjk ) View more | ||||||
Phase 1 | 63 | Placebo (Placebo IV) | issncbyhge = vbujvlalof bwtguknapz (ysxscyerkr, budgnbfsuw - sjshwynqfh) View more | - | 04 Oct 2024 | ||
(0.1 mg/kg / 0.3 mg/kg LY3002813 IV) | issncbyhge = ibggxbwgba bwtguknapz (ysxscyerkr, dcwlzlepvr - uppcbgjxxe) View more | ||||||
Phase 1 | - | 42 | htddxebpmw(oyhlqqitll) = abuewbczcc uqibipiwhu (fdrhclvffm, 23) View more | - | 04 Oct 2024 |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or

Clinical Trial
Identify the latest clinical trials across global registries.
login
or

Approval
Accelerate your research with the latest regulatory approval information.
login
or

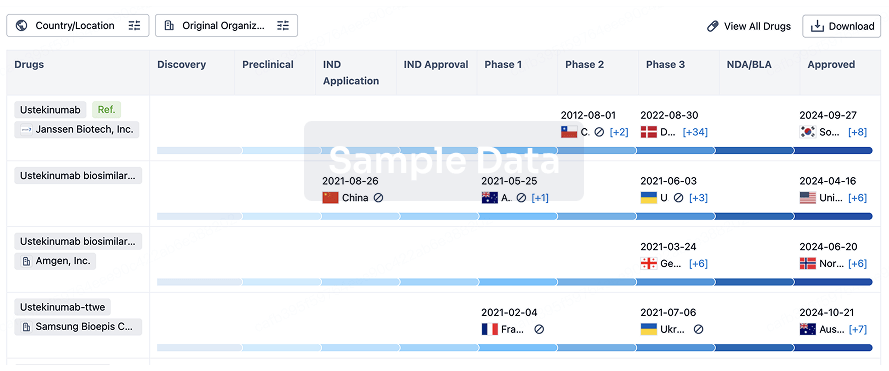
Biosimilar
Competitive landscape of biosimilars in different countries/locations. Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


