Request Demo
Last update 13 Dec 2025
Verosudil
Last update 13 Dec 2025
Overview
Basic Info
Drug Type Small molecule drug |
Synonyms Verosudil (USAN/INN), Verosudil Hydrochloride, AR-12286 + [1] |
Target |
Action inhibitors |
Mechanism ROCK inhibitors(Rho-associated kinases inhibitors) |
Therapeutic Areas |
Active Indication- |
Inactive Indication |
Originator Organization |
Active Organization- |
Inactive Organization |
License Organization- |
Drug Highest PhasePendingPhase 3 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Molecular FormulaC17H17N3O2S |
InChIKeyVDYRZXYYQMMFJW-UHFFFAOYSA-N |
CAS Registry1414854-42-4 |
Related
13
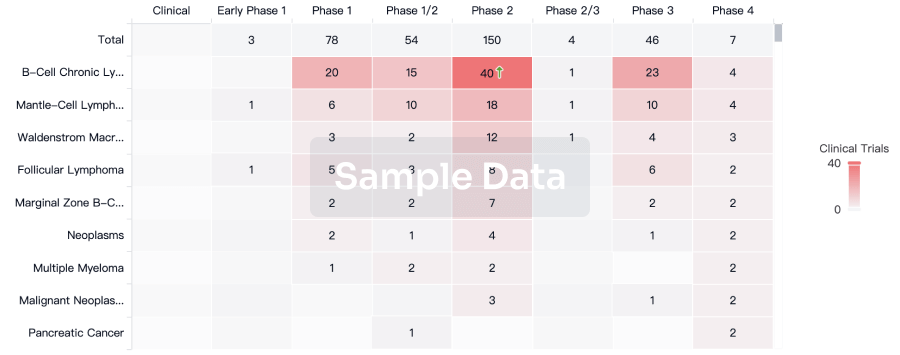
Clinical Trials associated with VerosudilCTRI/2024/04/065348
Safety and efficacy of rho-kinase inhibitor for treatment of postoperative striate keratopathy.
Start Date15 Apr 2024 |
Sponsor / Collaborator- |
NCT02173223
A Prospective Study to Assess the Hypotensive Efficacy of Rho-Kinase Inhibitor AR-12286 Ophthalmic Solution 0.5% and 0.7% in Patients With Uncontrolled Advanced Glaucoma With Prior Failed Trabeculectomy or Tube Shunt
A. To evaluate the ocular hypotensive efficacy of the rho-kinase Inhibitor (AR-12286 0.5% and 0.7%) ophthalmic solutions in glaucoma patients with failed prior glaucoma filtering surgery and uncontrolled IOP who are facing further surgical intervention. Patients will be treated for 6 months in this initial trial.
B. To evaluate the efficacy of AR-12286 in enabling treated patients to delay or avoid the necessity of further surgical intervention.
B. To evaluate the efficacy of AR-12286 in enabling treated patients to delay or avoid the necessity of further surgical intervention.
Start Date01 Jun 2014 |
Sponsor / Collaborator |
NCT02174991
A Prospective Study to Assess the Hypotensive Efficacy of Rho-Kinase Inhibitor AR-12286 Ophthalmic Solution 0.5% and 0.7% in Glaucoma Patients With Uncontrolled Intraocular Pressure to Avoid Surgical Intervention
A. To evaluate the ocular hypotensive efficacy of the rho-kinase Inhibitor (AR-12286 0.5% and 0.7%) ophthalmic solutions in open-angle glaucoma patients with uncontrolled IOP who are facing surgical intervention. Patients will be treated for 6 months in this initial trial.
B. To evaluate the efficacy of AR-12286 in enabling treated patients to delay or avoid the necessity of surgical intervention.
B. To evaluate the efficacy of AR-12286 in enabling treated patients to delay or avoid the necessity of surgical intervention.
Start Date01 Jun 2014 |
Sponsor / Collaborator |
100 Clinical Results associated with Verosudil
Login to view more data
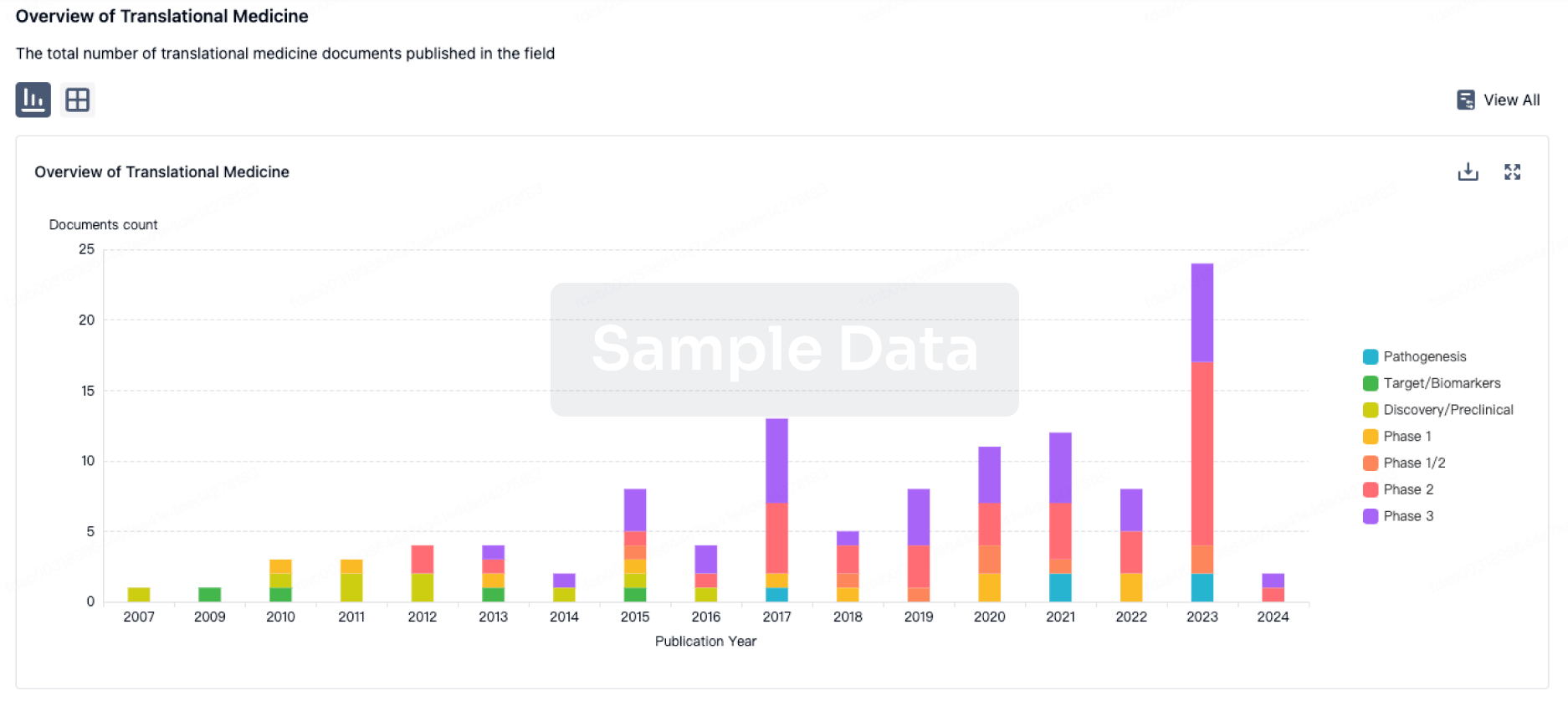
100 Translational Medicine associated with Verosudil
Login to view more data
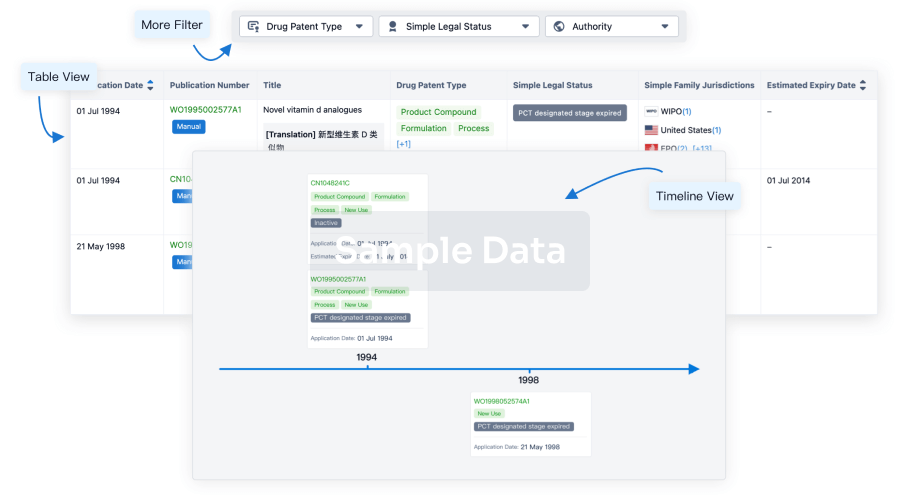
100 Patents (Medical) associated with Verosudil
Login to view more data
443
Literatures (Medical) associated with Verosudil01 Sep 2025·CRYOBIOLOGY
Corrigendum to “Ex vivo use of a Rho-kinase inhibitor during renal preservation improves graft function upon reperfusion” [Cryobiology 70 (2015) 71–75]
Author: Wohlschlaeger, Jeremias ; Kirchner, Carmen ; Lüer, Bastian ; Paul, Andreas ; Minor, Thomas ; Efferz, Patrik
01 Sep 2025·JAPANESE JOURNAL OF OPHTHALMOLOGY
Neuroprotective effect of ripasudil on retinal ganglion cells via an antioxidative mechanism
Article
Author: Yamagishi-Kimura, Reiko ; Honjo, Megumi ; Aihara, Makoto
Abstract:
Purpose:
To evaluate the neuroprotective effect of ripasudil, a rho-kinase inhibitor that is a commercially available glaucoma medication that lowers intraocular pressure. We explored the effects of ripasudil on retinal damage via oxidative stress (OS) in primary rat retinal ganglion cell (RGC) cultures and NMDA-induced retinal damage in mice.
Study design:
Experimental investigation
Methods:
Primary rat RGCs were isolated via a 2-step immunopanning method and cultured under normal cultivation conditions for 72 h and for a further 24 h in antioxidant-free medium for OS. We measured the number of living RGCs by use of calcein-AM and calpain activity via calpain immunoreactivity assays. Furthermore, we evaluated the effects of ripasudil via RGC counting in retinal flat-mounts from Thy1-CFP mice, retinal thickness via optical coherence tomography, and reduced glutathione levels via GSSG/GSH assays in NMDA-induced retinal damage.
Results:
The living RGC counts of normal, OS, 0.1, 1, 10, and 100 uM ripasudil under OS were 236.0 ± 21.6, 155.0 ± 13.2, 155.9 ± 17.1, 158.9 ± 12.0, 184.8 ± 26.9, and 201.1 ± 24.8 cells, respectively. 10 or 100 uM ripasudil significantly inhibited the OS-induced RGC reduction (P < 0.05 or 0.01). Furthermore, the enhanced calpain activity induced by OS was suppressed by 100 uM ripasudil (P < 0.05). In an in vivo study, the RGC counts in the NMDA-treated group were lower than those of the non-NMDA-treated group. NMDA-induced RGC loss was significantly suppressed by ripasudil (P < 0.01). Retinal thinning after 3 weeks of NMDA injection was also inhibited by ripasudil (P < 0.01 or 0.05). Furthermore, NMDA increased the glutathione level, whereas ripasudil suppressed it (P < 0.05).
Conclusions:
Ripasudil may have neuroprotective effects via an antioxidative mechanism, which could be useful as an intraocular pressure-independent additive.
01 Sep 2025·SURVEY OF OPHTHALMOLOGY
Exploring the potential of rho kinase inhibitors in ophthalmology: From mechanisms to clinical practice
Review
Author: Khaw, Peng Tee ; Tan, Jit Kai ; Ahmad, Sajjad ; Henein, Christin ; Steel, David H ; Viswanathan, Ananth ; Mathew, Rashmi G
INTRODUCTION:
The therapeutic potential of rho kinase (ROCK) inhibitors in ophthalmology is gaining attention, given their multifaceted role in cellular regulation, particularly within ocular pathologies. This review synthesizes findings from clinical and preclinical studies on the efficacy and safety of ROCK inhibitors across glaucoma, corneal, and retinal diseases. We performed a systematic database search in Ovid MEDLINE and Ovid Embase on 5th April 2022 using the following keywords: 'primary open angle glaucoma', 'glaucoma surgery', 'corneal wound healing', 'corneal endothelial dysfunction', 'diabetic retinopathy', 'diabetic macular oedema', 'age-related macular degeneration', 'rho kinase inhibitor', 'rho-kinase inhibitor', rock inhibitor', 'ripasudil', 'netarsudil' and 'fasudil'. Abstracts were screened for relevant studies and results summarized in tables. The analysis of trials done for ROCK inhibitors reveals that they are safe and efficacious drugs, demonstrating noninferiority to existing medical treatments and effective when combined with existing treatments, and are approved for use in treating glaucoma, but not corneal or retinal diseases. Questions remain, however, regarding optimal dosage, patient selection, and cost-effectiveness. ROCK inhibitors demonstrate significant efficacy in reducing intraocular pressure by improving aqueous humour outflow. Additionally, ROCK inhibitors show promise in enhancing endothelial cell migration, thus providing a novel treatment avenue for corneal diseases such as Fuchs endothelial dystrophy. In retinal conditions, including diabetic retinopathy and age-related macular degeneration, ROCK inhibitors reduce vascular permeability, inflammation, and fibrosis, stabilising disease progression.
2
News (Medical) associated with Verosudil10 Jan 2025
NEW YORK, Jan. 10, 2025 /PRNewswire/ -- Woolsey Pharmaceuticals, whose mission is to usher in a new era of neurodegenerative disease treatment, today announced that the U.S. Patent and Trademark Office (USPTO) has granted additional claims for the use of BRAVYL in treating ALS.
This latest patent allowance covers treatment of possible, probable laboratory-supported, probable, or definite ALS, as defined by El Escorial Revised ALS diagnostic criteria, using fasudil or its active metabolite. Further claims are directed to reducing neurofilament light (NfL). In Woolsey's REAL study of BRAVYL at 180mg/day, NfL was reduced by 15% from baseline to six months (p=0.0006). Data from the 300 mg/day REAL cohort is expected in June 2025.
Once issued, this patent will add to Woolsey's existing portfolio, which includes:
US Patent No. 11,779,588, covering the treatment of sporadic ALS with fasudil or its active metabolite;
US Patent No.12,128,053, covering treating (sporadic or familial) ALS using Woolsey's proprietary dysphagia-friendly formulation; and
US Patent Nos. 11,944,633 and 12,115,167, covering a range of dysphagia-friendly formulations of fasudil.
BRAVYL (oral fasudil), a Rho-kinase inhibitor, is an investigational drug believed to work by targeting cellular mechanisms that contribute to neuronal damage and dysfunction. Preclinical and clinical studies suggest that BRAVYL may reduce motor-neuron death, making it a promising candidate for ALS.
"These robust and strategically vital patent claims are part of a 36-patent-family portfolio we have developed for fasudil, a number of which have already issued," said Sven Jacobson, Chief Executive Officer of Woolsey Pharmaceuticals. "These newest patent claims further strengthen our proprietary position around the use of BRAVYL to treat ALS, and complement BRAVYL's ALS Orphan Drug Designations in both the U.S. and Europe."
About ALS
ALS is a fatal neurodegenerative disease characterized by inevitable, and often rapid, decline in patients as the disorder advances. Mean survival time is only two to five years. Accordingly, the ability to impede any worsening represents a meaningful advancement in efforts to enhance the prognosis and quality of life of individuals impacted by the devastating condition.
About Woolsey Pharmaceuticals:
New York-based Woolsey Pharmaceuticals, Inc. is a privately held, clinical-stage pharmaceutical company focused on developing and bringing lifesaving treatments to people affected by ALS and other neurodegenerative diseases.
SOURCE Woolsey Pharmaceuticals, Inc.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
Orphan Drug
09 Nov 2023
Endothelin receptor are G protein-coupled receptors (GPCRs) of the β-group of rhodopsin receptors that bind to endothelin ligands, which are 21 amino acid long peptides derived from longer prepro-endothelin precursors. There are at least four types known, ETA, ETB (ETB1, ETB2) and ETC. The ETA receptor is characterized by having high affinity and selectivity for ET-1 and ET-2 compared to ET-3, whereas the ETB receptor has equivalent high affinity for all three endothelin isopeptides.
Endothelin is a small molecule primarily secreted by vascular endothelium, with its receptors predominantly expressed in endothelial cells and vascular smooth muscle cells. Endothelin is related to cell proliferation and pulmonary vascular contraction. Research has reported that the concentration of endothelin in the serum of PAH patients is significantly increased, and the expression of endothelin receptors in vascular smooth muscle cells is overexpressed. The targets of endothelin receptor antagonists are endothelin receptors A and B.
Endothelin (ET) is divided into ET-1, ET-2, and ET-3. ET-1 is currently known as the most potent vasoconstrictor of vascular smooth muscle, and it is involved in maintaining normal blood pressure and promoting the proliferation of smooth muscle cells and endothelial cells. For endothelin A receptors, the affinity order of ET is ET-1 > ET-2 > ET-3; for endothelin B receptors, the affinity of the three ETs is equal. The A receptor is predominantly expressed in smooth muscle cells, and the B receptor is more abundant in endothelial cells. The vasoconstriction function of ET-1 is regulated by the A receptor, and the B receptor relaxes blood vessels by releasing nitric oxide.
Endothelins are synthesized in several tissues, including the vascular endothelium (ET-1 exclusively) and smooth muscle cells. Released endothelin binds to the endothelin receptors ETA and ETB, the ETA receptors on vascular smooth muscle cells mediating vasoconstriction, and the ETB receptors on the endothelium linked to nitric oxide (NO) and prostacyclin release.
Endothelin receptor Competitive LandscapeAccording to Patsnap Synapse, as of 13 Oct 2023, there are a total of 175 endothelin receptor drugs worldwide, from 97 organizations, covering 110 indications, and conducting 614 clinical trials..
👇Please click on the picture link below for free registration or login directly if you have freemium accounts, you can browse the latest research progress on drugs , indications, organizations, clinical trials, clinical results, and drug patents related to this target.
The current competitive landscape of the target endothelin receptor is characterized by the presence of multiple companies with drugs in various stages of development. Johnson & Johnson, GSK Plc, Idorsia Ltd., Pharmazz, Inc., and Gilead Sciences, Inc. are some of the companies with significant R&D progress in this area. The Approved phase has the highest number of drugs, indicating successful development and regulatory approval for specific indications such as Pulmonary Arterial Hypertension, Glomerulonephritis, IGA, and Subarachnoid Hemorrhage.
Small molecule drugs and Synthetic peptides are the most rapidly progressing drug types, suggesting potential competition around innovative drugs. Further analysis is required to determine the research and development institutions of these biosimilars.
The United States, Japan, and European Union are leading in terms of drug development under the target endothelin receptor. China has also made progress, although the number of drugs in development is relatively small compared to other countries.
Overall, the target endothelin receptor presents opportunities for further research and development, with potential for innovative drugs to address various indications and meet unmet medical needs
Vitreous Implant - PER-001 for the Treatment of Diabetic RetinopathyPER-001 is a small molecule drug that targets the endothelin receptor. It is being developed by Perfuse Therapeutics, Inc., a pharmaceutical company specializing in biomedicine. The drug is currently in Phase 2, which is the highest phase of clinical development globally.
PER-001 has shown potential therapeutic benefits in various therapeutic areas, including eye diseases, cardiovascular diseases, and endocrinology and metabolic diseases. Specifically, it has demonstrated efficacy in treating diabetic retinopathy, glaucoma (open-angle), and other related eye conditions.
👇Please click on the image below to directly access the latest data (R&D Status | Core Patent | Clinical Trial | Approval status in Global countries) of this drug.
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina, leading to vision impairment or even blindness. Glaucoma, on the other hand, is a group of eye conditions that damage the optic nerve, often caused by increased pressure in the eye. Open-angle glaucoma is the most common form of glaucoma, characterized by a gradual loss of peripheral vision.
The targeting of the endothelin receptor by PER-001 suggests that it may have a mechanism of action related to regulating blood vessel constriction and inflammation. This could potentially be beneficial in treating the aforementioned eye diseases, as well as cardiovascular diseases and endocrinology and metabolic diseases. However, further research and clinical trials are needed to fully understand the drug's efficacy and safety profile.
As PER-001 is currently in Phase 2, it indicates that the drug has already undergone initial safety testing and has shown promising results in early-stage clinical trials. Phase 2 trials typically involve a larger number of participants and aim to further evaluate the drug's effectiveness and side effects. If the drug continues to show positive results in Phase 2, it may progress to Phase 3 trials, which involve an even larger patient population and are crucial for obtaining regulatory approval.
In summary, PER-001 is a small molecule drug developed by Perfuse Therapeutics, Inc. that targets the endothelin receptor. It has shown potential in treating various eye diseases, including diabetic retinopathy and glaucoma (open-angle), as well as cardiovascular diseases and endocrinology and metabolic diseases. With its current status in Phase 2, further research and clinical trials will determine its potential as a therapeutic option in these therapeutic areas.
Clazosentan——Hope for Preventing Vasospasm after Subarachnoid Hemorrhage (SAH)Clazosentan is a small molecule drug that falls under the therapeutic areas of Nervous System Diseases and Cardiovascular Diseases. It specifically targets the ETA receptor. The drug is primarily indicated for the treatment of Subarachnoid Hemorrhage, Vasospasm, and Intracranial conditions.
Clazosentan was developed by F. Hoffmann-La Roche Ltd., a renowned pharmaceutical organization. As of the latest available information, the drug has reached the highest phase of approval globally. However, its highest phase in China is still pending.
👇Please click on the image below to directly access the latest data (R&D Status | Core Patent | Clinical Trial | Approval status in Global countries) of this drug.
The global first approval of Clazosentan took place in January 2022, with Japan being the country/location where it was first approved. It is important to note that Clazosentan is regulated as an orphan drug. Orphan drugs are medications developed to treat rare diseases or conditions that affect a small number of patients.
Aneurysmal subarachnoid hemorrhage (aSAH) is a sudden, life-threatening condition caused by the rupture of an aneurysm. It necessitates emergency surgery, including endovascular coiling or surgical microclipping, to prevent re-rupture. The dissolution of blood clots and the release of vasoconstrictive substances can induce cerebral vasospasm, typically commencing about 3 days after an aSAH attack, peaking on days 8-11, and subsiding on day 21.3. If left untreated, cerebral vasospasm may be a key factor in morbidity and mortality in patients with aSAH. Delayed ischemic neurological deficits (DIND), resulting from cerebral vasospasm, account for 17-40% of aSAH, and half of the patients with vasospasm develop cerebral infarction.
Nimodipine, a calcium channel blocker (administered orally or via intravenous injection), has become the standard treatment in the US and Europe for improving neurological prognosis following subarachnoid hemorrhage, but there is no convincing evidence that it affects the incidence of vasospasm or DIND. In Japan, intravenous fasudil hydrochloride (a Rho-kinase inhibitor) and intravenous ozagrel sodium (a thromboxane A2 synthase inhibitor) have been used to prevent vasospasm. However, the number of studies on these drugs is limited, and their impact on DIND and outcomes remains uncertain.
Endothelin-1 (ET-1) has potent and persistent vasoconstrictive effects. A large amount of ET-1 is produced after aSAH, making it a key factor in the development of cerebral vasospasm. Clazosentan is an endothelin receptor antagonist (ERA) that has been extensively studied for the prevention of cerebral vasospasm in patients with aSAH.
The CONSCIOUS-1 study demonstrated that Clazosentan reduces the incidence of moderate to severe vasospasm in patients with aSAH who have undergone aneurysm clamping or occlusion. This effect is dose-dependent, with a relative risk reduction (RRR) of up to 65%. Subsequent CONSCIOUS-2 and CONSCIOUS-3 trials investigated the impact of Clazosentan on the morbidity and all-cause mortality associated with cerebral vasospasm. CONSCIOUS-2 showed that Clazosentan at a dose of 5 mg/hour did not yield statistically significant treatment results, leading to the early termination of the CONSCIOUS-3 trial. However, an exploratory analysis of CONSCIOUS-3 indicated that the RRR of morbidity and all-cause mortality associated with cerebral vasospasm at a dose of 15 mg/hr Clazosentan was 44%. Meanwhile, a phase II exploratory dose study conducted in Japan and South Korea found that 10 mg/hr of Clazosentan, compared to placebo, reduced the morbidity and all-cause mortality associated with cerebral vasospasm in patients with aSAH who underwent surgical clamping. Its tolerability was also similar to that of 5 mg/hr.
In December 2022, Teiji Tominaga and colleagues from Japan published their research findings in J Neurosurg, assessing the impact of Clazosentan on the incidence of cerebral vasospasm-related morbidity and all-cause mortality in Japanese patients with aneurysmal subarachnoid hemorrhage (aSAH).
This involved two similar double-blind, placebo-controlled phase III trials involving aSAH patients, accomplished by 57 Japanese centers. One trial enrolled aSAH patients with intravascular coil embolization of aneurysms, while another included aSAH patients who had undergone surgical clipping of aneurysms. In each study, Clazosentan (10mg/hr) or placebo (1:1) was randomly administered intravenously within 48 hours of SAH onset and continued until day 15. Stratification was based on the WFNS grading. The primary endpoints of each trial were the incidence of cerebral vasospasm-related morbidity and all-cause mortality within 6 weeks of aSAH, including new-onset cerebral infarction, delayed ischemic neurological deficit, and all-cause mortality.
In summary, Clazosentan is a small molecule drug developed by F. Hoffmann-La Roche Ltd. It targets the ETA receptor and is indicated for the treatment of Subarachnoid Hemorrhage, Vasospasm, and Intracranial conditions. The drug has reached the highest phase of approval globally and is regulated as an orphan drug. Its first approval occurred in Japan in January 2022. However, its highest phase in China is still pending.
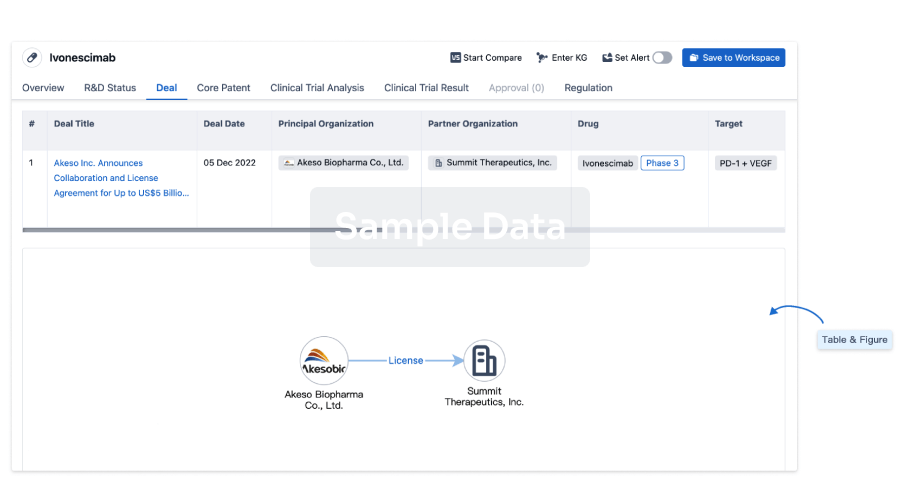
100 Deals associated with Verosudil
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Ocular Hypertension | Phase 3 | - | - | |
| Glaucoma | Phase 2 | United States | 01 Feb 2010 | |
| Glaucoma, Open-Angle | Phase 2 | United States | 01 May 2009 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
Phase 2 | 10 | awtiqwcjzv(smeldcjgrs) = ladfcxvbfr fskbivtpfd (xxlkkhgqmp ) View more | Positive | 01 Sep 2016 | |||
Phase 2 | 10 | (0.5%) | hmcjtnuryj(hnklmttrey) = vpnolfsnyq wskuosawww (jogauypepd, 2.4) View more | - | 24 Apr 2015 | ||
(0.7%) | hmcjtnuryj(hnklmttrey) = jvhjycoyqh wskuosawww (jogauypepd, 2.4) View more | ||||||
Phase 2 | 89 | xgtgzheyvw(ksqdsnnyrp) = xrrjjqjrkw whrsauyzya (jjpyecmzrf ) View more | Positive | 01 Nov 2011 | |||
xgtgzheyvw(ksqdsnnyrp) = iovrppvift whrsauyzya (jjpyecmzrf ) View more | |||||||
Phase 1 | - | 18 | tdeqncuwfw(jmwkhjobeh) = trace to moderate conjunctival hyperemia that gradually returned to baseline by 8 hrs after dosing zgjntwmwdy (apabxriffy ) | Positive | 01 Apr 2011 |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
Approval
Accelerate your research with the latest regulatory approval information.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

