Request Demo
Last update 08 May 2025
TGM3
Last update 08 May 2025
Basic Info
Synonyms Protein-glutamine gamma-glutamyltransferase E, Protein-glutamine gamma-glutamyltransferase E 27 kDa non-catalytic chain, Protein-glutamine gamma-glutamyltransferase E 50 kDa catalytic chain + [8] |
Introduction Catalyzes the calcium-dependent formation of isopeptide cross-links between glutamine and lysine residues in various proteins, as well as the conjugation of polyamines to proteins. Involved in the formation of the cornified envelope (CE), a specialized component consisting of covalent cross-links of proteins beneath the plasma membrane of terminally differentiated keratinocytes. Catalyzes small proline-rich proteins (SPRR1 and SPRR2) and LOR cross-linking to form small interchain oligomers, which are further cross-linked by TGM1 onto the growing CE scaffold (By similarity). In hair follicles, involved in cross-linking structural proteins to hardening the inner root sheath. |
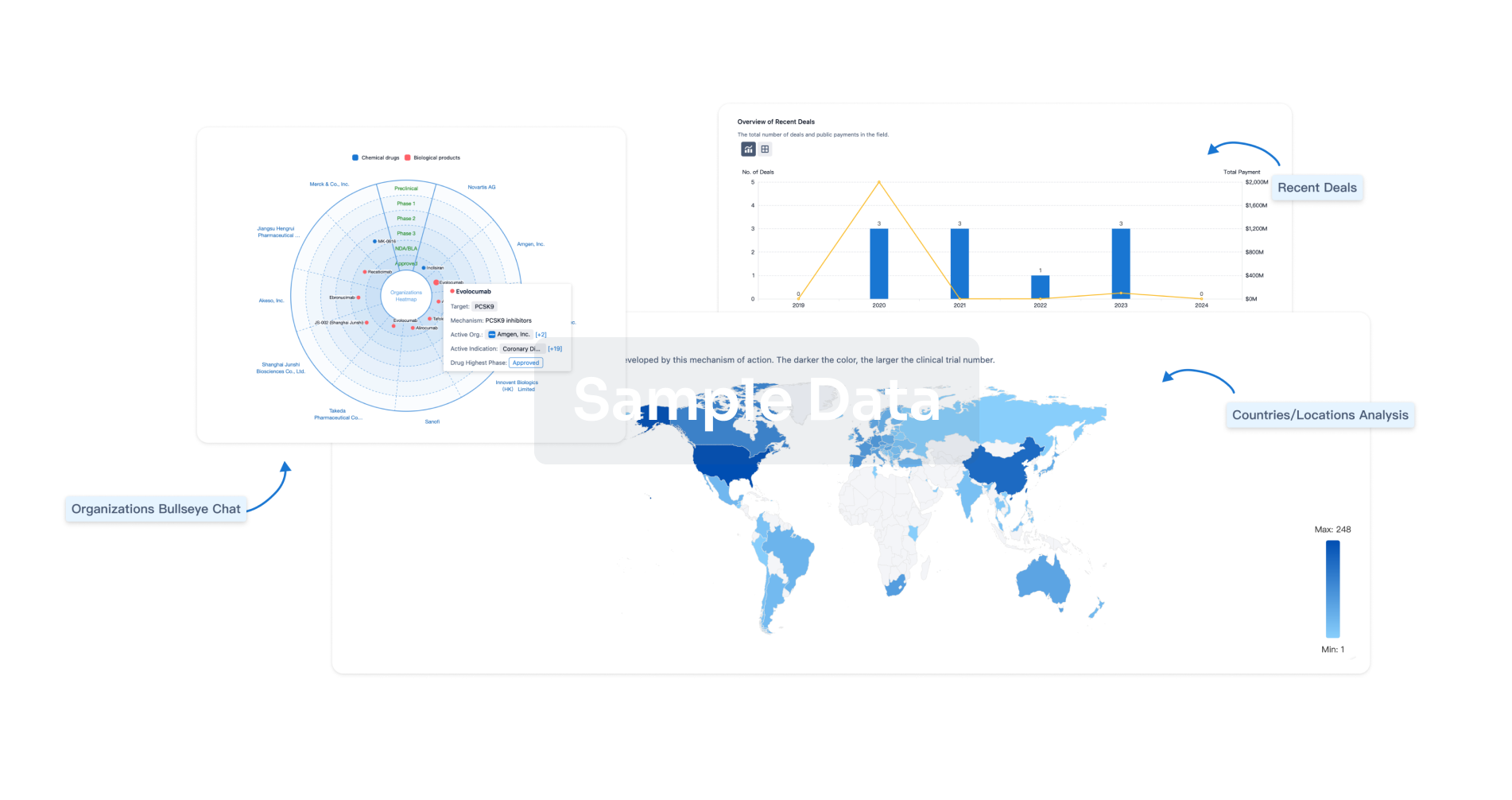
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
