Request Demo
Last update 01 Nov 2024
IL-12R x RIG-I
Last update 01 Nov 2024
Related
1
Drugs associated with IL-12R x RIG-ITarget |
Mechanism IL-12R stimulants [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePhase 1/2 |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
1
Clinical Trials associated with IL-12R x RIG-INCT04752722
A Phase 1/2 Study of EG-70 as an Intravesical Administration to Patients With BCG Unresponsive Non-Muscle Invasive Bladder Cancer (NMIBC) and High-Risk NMIBC Patients Who Are BCG Naïve or Received Incomplete BCG Treatment
This study will evaluate the safety and efficacy of intravesical administration of EG-70 in the bladder and its effect on bladder tumors in patients with NMIBC.
This study study consists of two phases; a Phase 1 dose-escalation to establish safety and recommended the phase 2 dose, followed by a Phase 2 study to establish how effective the treatment is.
The Study will include patients with NMIBC with Cis for whom BCG therapy is unresponsive and patients with NMIBC with Cis who are BCG-naïve or inadequately treated.
This study study consists of two phases; a Phase 1 dose-escalation to establish safety and recommended the phase 2 dose, followed by a Phase 2 study to establish how effective the treatment is.
The Study will include patients with NMIBC with Cis for whom BCG therapy is unresponsive and patients with NMIBC with Cis who are BCG-naïve or inadequately treated.
Start Date22 Apr 2021 |
Sponsor / Collaborator |
100 Clinical Results associated with IL-12R x RIG-I
Login to view more data
100 Translational Medicine associated with IL-12R x RIG-I
Login to view more data
0 Patents (Medical) associated with IL-12R x RIG-I
Login to view more data
5
Literatures (Medical) associated with IL-12R x RIG-I01 Jan 2022·The Immunogenetics of Dermatologic DiseasesQ4 · MEDICINE
The Immunogenetics of Psoriasis
Q4 · MEDICINE
Article
Author: Cinotti, Elisa ; Rubegni, Pietro ; Trovato, Emanuele
01 May 2021·Brain PathologyQ1 · MEDICINE
NanoString technology distinguishes anti‐TIF‐1γ+ from anti‐Mi‐2+ dermatomyositis patients
Q1 · MEDICINE
Article
Author: Koll, Randi ; Schänzer, Anne ; Schneider, Udo ; Eede, Pascale ; Freitag, Kiara ; Froehlich, Waltraud ; Radke, Josefine ; Benveniste, Olivier ; Allenbach, Yves ; Heinzeling, Lucie ; Stenzel, Werner ; Goebel, Hans‐Hilmar ; Preusse, Corinna
01 Nov 2015·Journal of AutoimmunityQ1 · MEDICINE
The immunogenetics of Psoriasis: A comprehensive review
Q1 · MEDICINE
Review
Author: Krueger, James G ; Bowcock, Anne M ; Harden, Jamie L
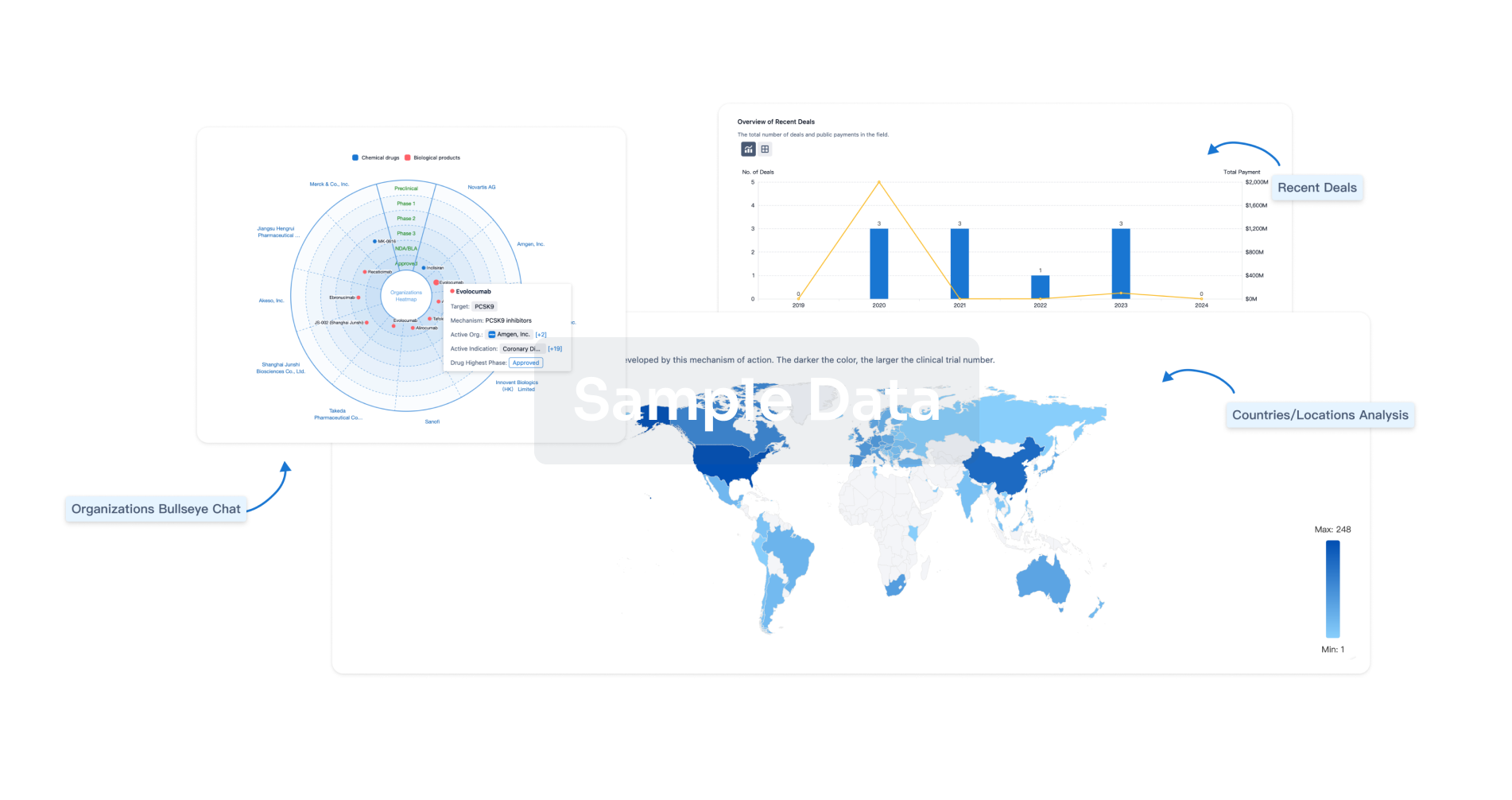
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
