Request Demo
What is Amoxapine used for?
15 June 2024
Amoxapine is a tricyclic antidepressant (TCA) that has been around for several decades, making its debut in the pharmaceutical market in the 1970s. Marketed under trade names such as Asendin, Defanyl, and Demolox, it has found its place predominantly in the treatment of major depressive disorder (MDD). Developed initially by research institutions focused on mental health, Amoxapine was engineered to target neurotransmitter imbalances in the brain that are believed to contribute to depression. While it has been somewhat overshadowed by newer classes of antidepressants like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), Amoxapine remains an important option for certain patient populations. It is particularly noted for its ability to also address psychotic symptoms, offering a dual mechanism of action that sets it apart from some other antidepressants.
Amoxapine is classified as a secondary amine TCA, distinguishing it from tertiary amines by its somewhat different side effect profile and mechanism of action. The drug is indicated primarily for major depressive disorder but has also shown efficacy in treating anxiety disorders and, in some cases, as an adjunct treatment for schizophrenia. The ongoing research into Amoxapine aims to refine its usage guidelines, manage its side effects better, and explore its potential benefits in other psychiatric conditions.
Amoxapine Mechanism of Action
Amoxapine's mechanism of action is multifaceted, contributing to its efficacy in treating both depressive and psychotic symptoms. At its core, Amoxapine works by inhibiting the reuptake of two key neurotransmitters: norepinephrine and serotonin. By blocking the reuptake of these neurotransmitters into presynaptic neurons, Amoxapine increases their availability in the synaptic cleft, thus enhancing neurotransmission and improving mood and affective symptoms.
What sets Amoxapine apart from other TCAs is its ability to antagonize dopamine receptors, particularly the D2 and D3 receptors. This dopamine receptor antagonism is akin to the action of some antipsychotic medications, which explains why Amoxapine can be effective in managing psychotic symptoms such as hallucinations and delusions. The dual action on both norepinephrine/serotonin reuptake inhibition and dopamine receptor antagonism gives Amoxapine a unique profile that can be particularly beneficial for patients with complex psychiatric conditions.
How to Use Amoxapine
Amoxapine is typically administered orally in the form of tablets. The dosage can vary widely depending on the severity of the condition being treated, patient response, and other factors such as age and kidney function. The initial dose for adults generally starts at 50 mg two to three times daily, with the potential to increase gradually up to a maximum of 300 mg per day, divided into multiple doses.
The onset of action for Amoxapine can be somewhat variable. Some patients may begin to notice an improvement in their symptoms within a week, although it may take up to four weeks for the full therapeutic effects to be realized. It is crucial for patients to adhere to their prescribed regimen and not to discontinue the medication abruptly, as doing so can lead to withdrawal symptoms and a potential relapse of depressive symptoms.
In cases where a rapid therapeutic response is required, clinicians may opt to initiate treatment with a higher dose, closely monitoring the patient for any adverse reactions. Elderly patients usually require lower doses to minimize the risk of side effects, and dose adjustments are similarly made for individuals with renal or hepatic impairments.
What is Amoxapine Side Effects
Like all medications, Amoxapine is associated with a range of potential side effects. The side effects can be broadly categorized into common, less common, and rare but serious. Common side effects include drowsiness, dry mouth, constipation, and blurred vision. These are typically dose-dependent and may subside as the body adjusts to the medication. However, persistent side effects should be reported to a healthcare provider.
Less common side effects of Amoxapine include weight gain, orthostatic hypotension (a drop in blood pressure upon standing), and sexual dysfunction. These can be troubling for patients and may warrant a re-evaluation of the treatment regimen. Of particular concern are the potential cardiovascular effects, such as arrhythmias and tachycardia, which necessitate cautious use in patients with preexisting heart conditions.
Rare but serious side effects include neuroleptic malignant syndrome (NMS), a potentially life-threatening condition characterized by high fever, muscle rigidity, and autonomic dysfunction. Another serious condition to be aware of is tardive dyskinesia, which involves involuntary, repetitive movements and is more commonly associated with long-term use of dopamine antagonists.
Contraindications for Amoxapine include a history of hypersensitivity to tricyclic antidepressants, recent myocardial infarction, and concurrent use of monoamine oxidase inhibitors (MAOIs). It is also contraindicated in patients with a known predisposition to seizure disorders, as Amoxapine can lower the seizure threshold.
What Other Drugs Will Affect Amoxapine
Amoxapine interacts with a variety of other medications, which can either enhance its effects or increase the risk of adverse reactions. One of the most critical interactions is with monoamine oxidase inhibitors (MAOIs). Combining Amoxapine with MAOIs can result in severe, life-threatening reactions, including hypertensive crises and serotonin syndrome. A minimum two-week washout period is recommended when transitioning between these medications.
Concomitant use of other central nervous system depressants, such as alcohol, benzodiazepines, and opioids, can potentiate the sedative effects of Amoxapine, increasing the risk of drowsiness, confusion, and respiratory depression. Likewise, combining Amoxapine with antihistamines or other anticholinergic agents can exacerbate anticholinergic side effects like dry mouth, blurred vision, and constipation.
Amoxapine can also interact with medications that affect the cytochrome P450 enzyme system, particularly CYP2D6. Drugs that inhibit CYP2D6, such as certain SSRIs (e.g., fluoxetine, paroxetine), can increase the plasma concentration of Amoxapine, raising the risk of toxicity. Conversely, inducers of this enzyme system, such as rifampin and carbamazepine, can decrease Amoxapine levels, potentially reducing its therapeutic efficacy.
Patients taking antihypertensive medications should be monitored closely, as Amoxapine can counteract the blood pressure-lowering effects of these drugs. Moreover, Amoxapine’s cardiovascular side effects necessitate caution when used alongside other medications that can affect heart rhythm or blood pressure.
In conclusion, while Amoxapine remains a valuable option in the treatment of major depressive disorder and psychotic symptoms, its use requires careful consideration of its side effect profile and potential drug interactions. Regular monitoring by healthcare providers and open communication with patients are essential to maximize the benefits of Amoxapine while minimizing its risks.
Amoxapine is classified as a secondary amine TCA, distinguishing it from tertiary amines by its somewhat different side effect profile and mechanism of action. The drug is indicated primarily for major depressive disorder but has also shown efficacy in treating anxiety disorders and, in some cases, as an adjunct treatment for schizophrenia. The ongoing research into Amoxapine aims to refine its usage guidelines, manage its side effects better, and explore its potential benefits in other psychiatric conditions.
Amoxapine Mechanism of Action
Amoxapine's mechanism of action is multifaceted, contributing to its efficacy in treating both depressive and psychotic symptoms. At its core, Amoxapine works by inhibiting the reuptake of two key neurotransmitters: norepinephrine and serotonin. By blocking the reuptake of these neurotransmitters into presynaptic neurons, Amoxapine increases their availability in the synaptic cleft, thus enhancing neurotransmission and improving mood and affective symptoms.
What sets Amoxapine apart from other TCAs is its ability to antagonize dopamine receptors, particularly the D2 and D3 receptors. This dopamine receptor antagonism is akin to the action of some antipsychotic medications, which explains why Amoxapine can be effective in managing psychotic symptoms such as hallucinations and delusions. The dual action on both norepinephrine/serotonin reuptake inhibition and dopamine receptor antagonism gives Amoxapine a unique profile that can be particularly beneficial for patients with complex psychiatric conditions.
How to Use Amoxapine
Amoxapine is typically administered orally in the form of tablets. The dosage can vary widely depending on the severity of the condition being treated, patient response, and other factors such as age and kidney function. The initial dose for adults generally starts at 50 mg two to three times daily, with the potential to increase gradually up to a maximum of 300 mg per day, divided into multiple doses.
The onset of action for Amoxapine can be somewhat variable. Some patients may begin to notice an improvement in their symptoms within a week, although it may take up to four weeks for the full therapeutic effects to be realized. It is crucial for patients to adhere to their prescribed regimen and not to discontinue the medication abruptly, as doing so can lead to withdrawal symptoms and a potential relapse of depressive symptoms.
In cases where a rapid therapeutic response is required, clinicians may opt to initiate treatment with a higher dose, closely monitoring the patient for any adverse reactions. Elderly patients usually require lower doses to minimize the risk of side effects, and dose adjustments are similarly made for individuals with renal or hepatic impairments.
What is Amoxapine Side Effects
Like all medications, Amoxapine is associated with a range of potential side effects. The side effects can be broadly categorized into common, less common, and rare but serious. Common side effects include drowsiness, dry mouth, constipation, and blurred vision. These are typically dose-dependent and may subside as the body adjusts to the medication. However, persistent side effects should be reported to a healthcare provider.
Less common side effects of Amoxapine include weight gain, orthostatic hypotension (a drop in blood pressure upon standing), and sexual dysfunction. These can be troubling for patients and may warrant a re-evaluation of the treatment regimen. Of particular concern are the potential cardiovascular effects, such as arrhythmias and tachycardia, which necessitate cautious use in patients with preexisting heart conditions.
Rare but serious side effects include neuroleptic malignant syndrome (NMS), a potentially life-threatening condition characterized by high fever, muscle rigidity, and autonomic dysfunction. Another serious condition to be aware of is tardive dyskinesia, which involves involuntary, repetitive movements and is more commonly associated with long-term use of dopamine antagonists.
Contraindications for Amoxapine include a history of hypersensitivity to tricyclic antidepressants, recent myocardial infarction, and concurrent use of monoamine oxidase inhibitors (MAOIs). It is also contraindicated in patients with a known predisposition to seizure disorders, as Amoxapine can lower the seizure threshold.
What Other Drugs Will Affect Amoxapine
Amoxapine interacts with a variety of other medications, which can either enhance its effects or increase the risk of adverse reactions. One of the most critical interactions is with monoamine oxidase inhibitors (MAOIs). Combining Amoxapine with MAOIs can result in severe, life-threatening reactions, including hypertensive crises and serotonin syndrome. A minimum two-week washout period is recommended when transitioning between these medications.
Concomitant use of other central nervous system depressants, such as alcohol, benzodiazepines, and opioids, can potentiate the sedative effects of Amoxapine, increasing the risk of drowsiness, confusion, and respiratory depression. Likewise, combining Amoxapine with antihistamines or other anticholinergic agents can exacerbate anticholinergic side effects like dry mouth, blurred vision, and constipation.
Amoxapine can also interact with medications that affect the cytochrome P450 enzyme system, particularly CYP2D6. Drugs that inhibit CYP2D6, such as certain SSRIs (e.g., fluoxetine, paroxetine), can increase the plasma concentration of Amoxapine, raising the risk of toxicity. Conversely, inducers of this enzyme system, such as rifampin and carbamazepine, can decrease Amoxapine levels, potentially reducing its therapeutic efficacy.
Patients taking antihypertensive medications should be monitored closely, as Amoxapine can counteract the blood pressure-lowering effects of these drugs. Moreover, Amoxapine’s cardiovascular side effects necessitate caution when used alongside other medications that can affect heart rhythm or blood pressure.
In conclusion, while Amoxapine remains a valuable option in the treatment of major depressive disorder and psychotic symptoms, its use requires careful consideration of its side effect profile and potential drug interactions. Regular monitoring by healthcare providers and open communication with patients are essential to maximize the benefits of Amoxapine while minimizing its risks.
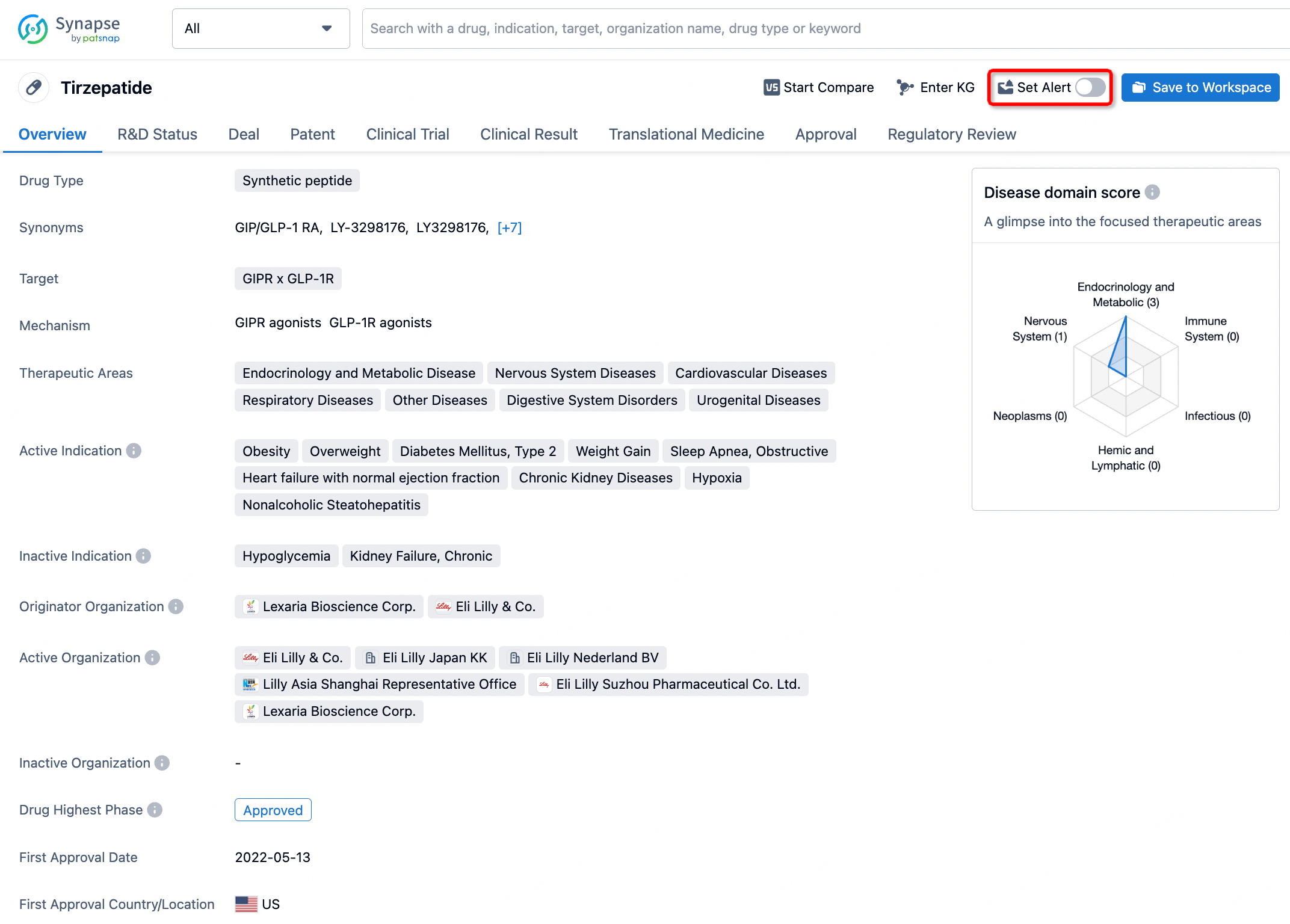
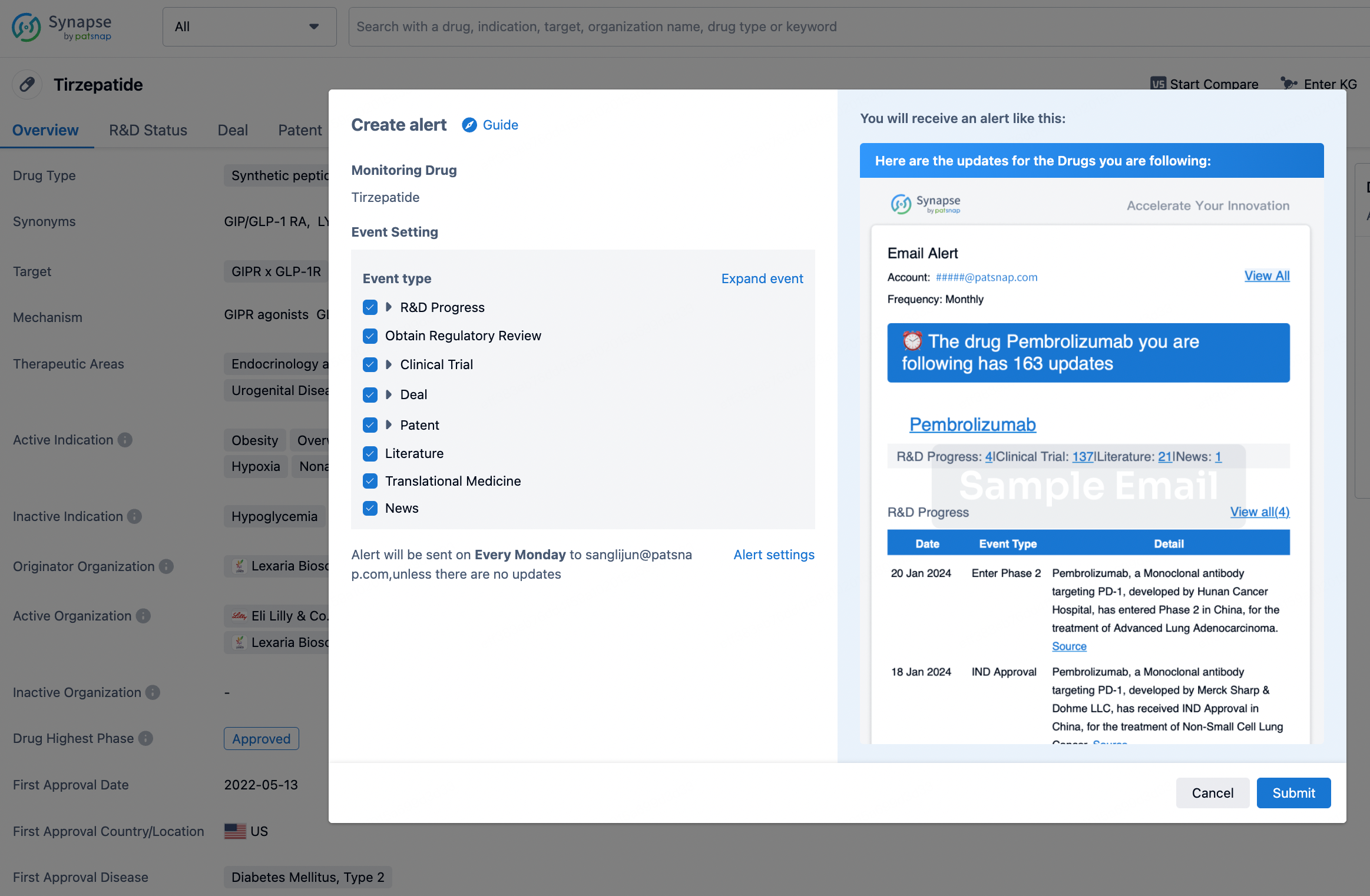
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.