Request Demo
What is Fludarabine Phosphate used for?
14 June 2024
Fludarabine Phosphate is a chemotherapeutic agent with a well-established history of use in the treatment of certain types of cancer. Known by its trade names such as Fludara, this drug is particularly effective in targeting chronic lymphocytic leukemia (CLL) and other hematologic malignancies. Developed and researched extensively, fludarabine phosphate has been a mainstay in therapeutic regimens managed by institutions worldwide, including the National Cancer Institute (NCI) and major pharmaceutical companies.
This purine analog belongs to the class of antimetabolites, which interfere with DNA synthesis and function. Fludarabine phosphate is indicated not just for CLL but also for low-grade non-Hodgkin's lymphoma and acute myeloid leukemia (AML) in certain cases, often as part of combination therapy. Its research progress has been notable, with numerous clinical studies confirming its efficacy and exploring new applications.
Fludarabine phosphate’s mechanism of action is multifaceted, involving the inhibition of DNA synthesis. Once administered, it is rapidly dephosphorylated to 2-fluoro-ara-A, an active metabolite. Subsequently, this metabolite is phosphorylated intracellularly by deoxycytidine kinase to its triphosphate form, 2-fluoro-ara-ATP. This active triphosphate form competes with deoxyadenosine triphosphate (dATP) for incorporation into the DNA strand during synthesis. Incorporation of 2-fluoro-ara-ATP into the DNA leads to chain termination. Furthermore, it inhibits ribonucleotide reductase, an enzyme critical for the generation of deoxynucleotides for DNA synthesis, thus further impeding cell proliferation. This disruption particularly targets rapidly dividing cells, such as malignant leukocytes, leading to apoptosis or programmed cell death.
Fludarabine phosphate is typically administered intravenously, though oral formulations are also available. Intravenous administration involves a precise dosing regimen often delivered over a course of five consecutive days, repeated every 28 days. The onset of action varies, but therapeutic effects are usually observable within a few treatment cycles. The drug is administered in a clinical setting to monitor for any adverse reactions, ensuring that appropriate supportive care is available if needed.
Patients undergoing fludarabine phosphate treatment are meticulously dosed based on body surface area, typically at 25 mg/m²/day. The drug is infused over 30 minutes to avoid rapid fluctuations in blood concentration, which could provoke adverse reactions. Oral administration, on the other hand, offers more convenience and can be taken at home, though close monitoring remains crucial.
As with any potent chemotherapeutic agent, fludarabine phosphate has a range of side effects that must be considered. Common side effects include myelosuppression, which manifests as decreased levels of white blood cells, red blood cells, and platelets, leading to an increased risk of infection, anemia, and bleeding, respectively. Other notable side effects include nausea, vomiting, diarrhea, and fatigue. Patients may also experience fever, cough, and dyspnea, indicative of possible infections or pulmonary complications.
Serious but less common side effects include neurotoxicity, which can present as confusion, seizures, and even coma, particularly at high doses. Tumor lysis syndrome, a condition resulting from the rapid destruction of malignant cells, can lead to acute renal failure and requires prompt intervention. Additionally, patients treated with fludarabine phosphate are at heightened risk for opportunistic infections due to immunosuppression, necessitating prophylactic antimicrobials and vigilant monitoring.
Contradictions for the use of fludarabine phosphate include severe renal impairment, as the drug is primarily excreted via the kidneys. Patients with a history of severe hypersensitivity to fludarabine phosphate or any of its components should avoid its use. Caution is also advised in patients with pre-existing neurological disorders due to the risk of exacerbation.
The effects of other drugs on fludarabine phosphate pharmacokinetics and pharmacodynamics are significant and should be carefully managed. For instance, concomitant use of pentostatin is contraindicated due to an increased risk of severe pulmonary toxicity. Immunosuppressive agents, such as cyclosporine and tacrolimus, may potentiate the immunosuppressive effects of fludarabine phosphate, increasing the risk of infections.
Non-steroidal anti-inflammatory drugs (NSAIDs) and other nephrotoxic agents can exacerbate renal toxicity, necessitating close monitoring of renal function. Additionally, live vaccines are contraindicated during and after treatment with fludarabine phosphate, due to the risk of disseminated infection secondary to immunosuppression.
In conclusion, fludarabine phosphate is a potent chemotherapeutic agent with specific indications and a well-characterized mechanism of action. Its administration requires careful dosing and monitoring to manage its potentially severe side effects and interactions with other medications. While highly effective in treating certain hematologic malignancies, it necessitates a comprehensive understanding of its pharmacological profile to optimize outcomes and minimize risks for patients.
This purine analog belongs to the class of antimetabolites, which interfere with DNA synthesis and function. Fludarabine phosphate is indicated not just for CLL but also for low-grade non-Hodgkin's lymphoma and acute myeloid leukemia (AML) in certain cases, often as part of combination therapy. Its research progress has been notable, with numerous clinical studies confirming its efficacy and exploring new applications.
Fludarabine phosphate’s mechanism of action is multifaceted, involving the inhibition of DNA synthesis. Once administered, it is rapidly dephosphorylated to 2-fluoro-ara-A, an active metabolite. Subsequently, this metabolite is phosphorylated intracellularly by deoxycytidine kinase to its triphosphate form, 2-fluoro-ara-ATP. This active triphosphate form competes with deoxyadenosine triphosphate (dATP) for incorporation into the DNA strand during synthesis. Incorporation of 2-fluoro-ara-ATP into the DNA leads to chain termination. Furthermore, it inhibits ribonucleotide reductase, an enzyme critical for the generation of deoxynucleotides for DNA synthesis, thus further impeding cell proliferation. This disruption particularly targets rapidly dividing cells, such as malignant leukocytes, leading to apoptosis or programmed cell death.
Fludarabine phosphate is typically administered intravenously, though oral formulations are also available. Intravenous administration involves a precise dosing regimen often delivered over a course of five consecutive days, repeated every 28 days. The onset of action varies, but therapeutic effects are usually observable within a few treatment cycles. The drug is administered in a clinical setting to monitor for any adverse reactions, ensuring that appropriate supportive care is available if needed.
Patients undergoing fludarabine phosphate treatment are meticulously dosed based on body surface area, typically at 25 mg/m²/day. The drug is infused over 30 minutes to avoid rapid fluctuations in blood concentration, which could provoke adverse reactions. Oral administration, on the other hand, offers more convenience and can be taken at home, though close monitoring remains crucial.
As with any potent chemotherapeutic agent, fludarabine phosphate has a range of side effects that must be considered. Common side effects include myelosuppression, which manifests as decreased levels of white blood cells, red blood cells, and platelets, leading to an increased risk of infection, anemia, and bleeding, respectively. Other notable side effects include nausea, vomiting, diarrhea, and fatigue. Patients may also experience fever, cough, and dyspnea, indicative of possible infections or pulmonary complications.
Serious but less common side effects include neurotoxicity, which can present as confusion, seizures, and even coma, particularly at high doses. Tumor lysis syndrome, a condition resulting from the rapid destruction of malignant cells, can lead to acute renal failure and requires prompt intervention. Additionally, patients treated with fludarabine phosphate are at heightened risk for opportunistic infections due to immunosuppression, necessitating prophylactic antimicrobials and vigilant monitoring.
Contradictions for the use of fludarabine phosphate include severe renal impairment, as the drug is primarily excreted via the kidneys. Patients with a history of severe hypersensitivity to fludarabine phosphate or any of its components should avoid its use. Caution is also advised in patients with pre-existing neurological disorders due to the risk of exacerbation.
The effects of other drugs on fludarabine phosphate pharmacokinetics and pharmacodynamics are significant and should be carefully managed. For instance, concomitant use of pentostatin is contraindicated due to an increased risk of severe pulmonary toxicity. Immunosuppressive agents, such as cyclosporine and tacrolimus, may potentiate the immunosuppressive effects of fludarabine phosphate, increasing the risk of infections.
Non-steroidal anti-inflammatory drugs (NSAIDs) and other nephrotoxic agents can exacerbate renal toxicity, necessitating close monitoring of renal function. Additionally, live vaccines are contraindicated during and after treatment with fludarabine phosphate, due to the risk of disseminated infection secondary to immunosuppression.
In conclusion, fludarabine phosphate is a potent chemotherapeutic agent with specific indications and a well-characterized mechanism of action. Its administration requires careful dosing and monitoring to manage its potentially severe side effects and interactions with other medications. While highly effective in treating certain hematologic malignancies, it necessitates a comprehensive understanding of its pharmacological profile to optimize outcomes and minimize risks for patients.
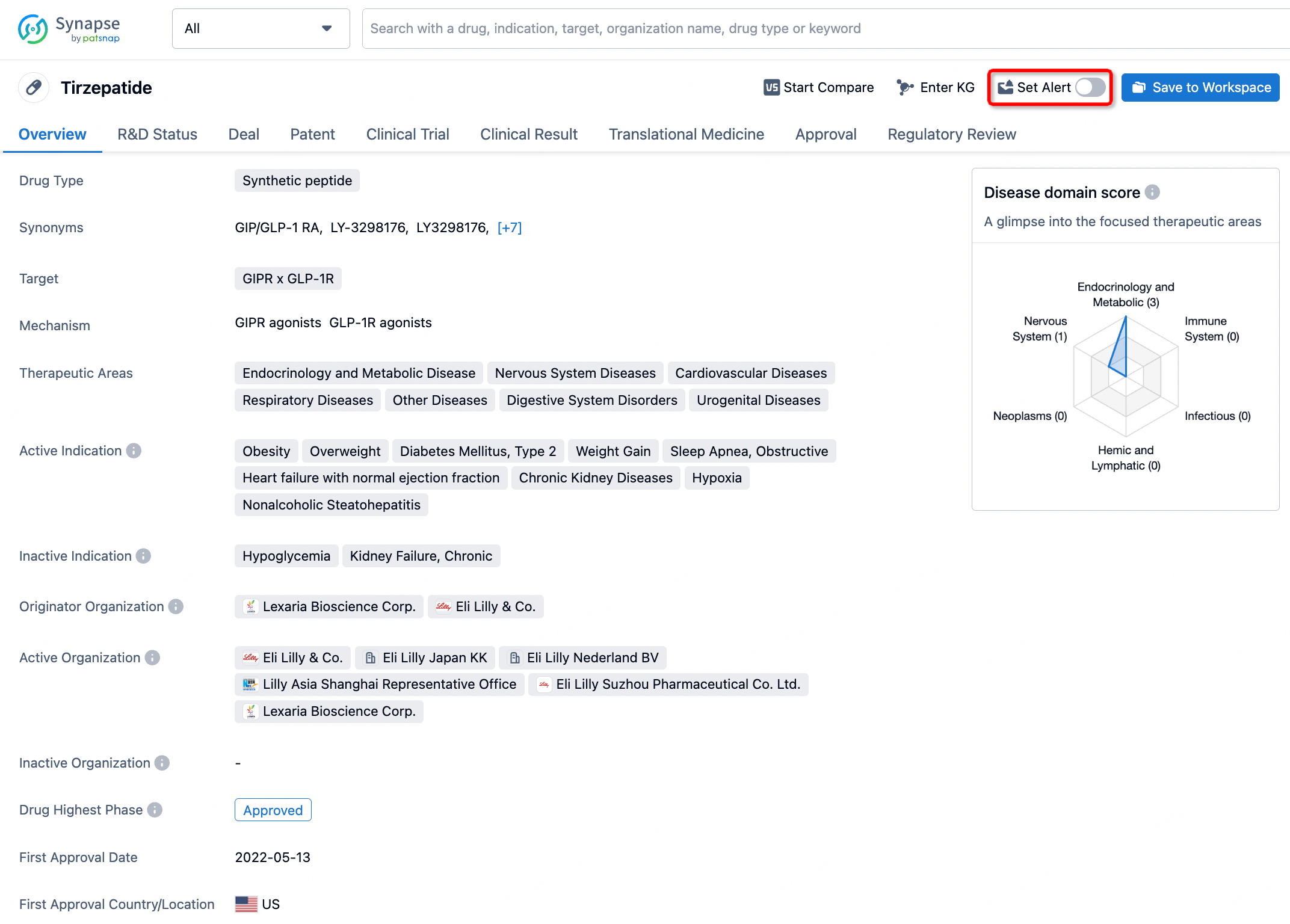
How to obtain the latest development progress of all drugs?
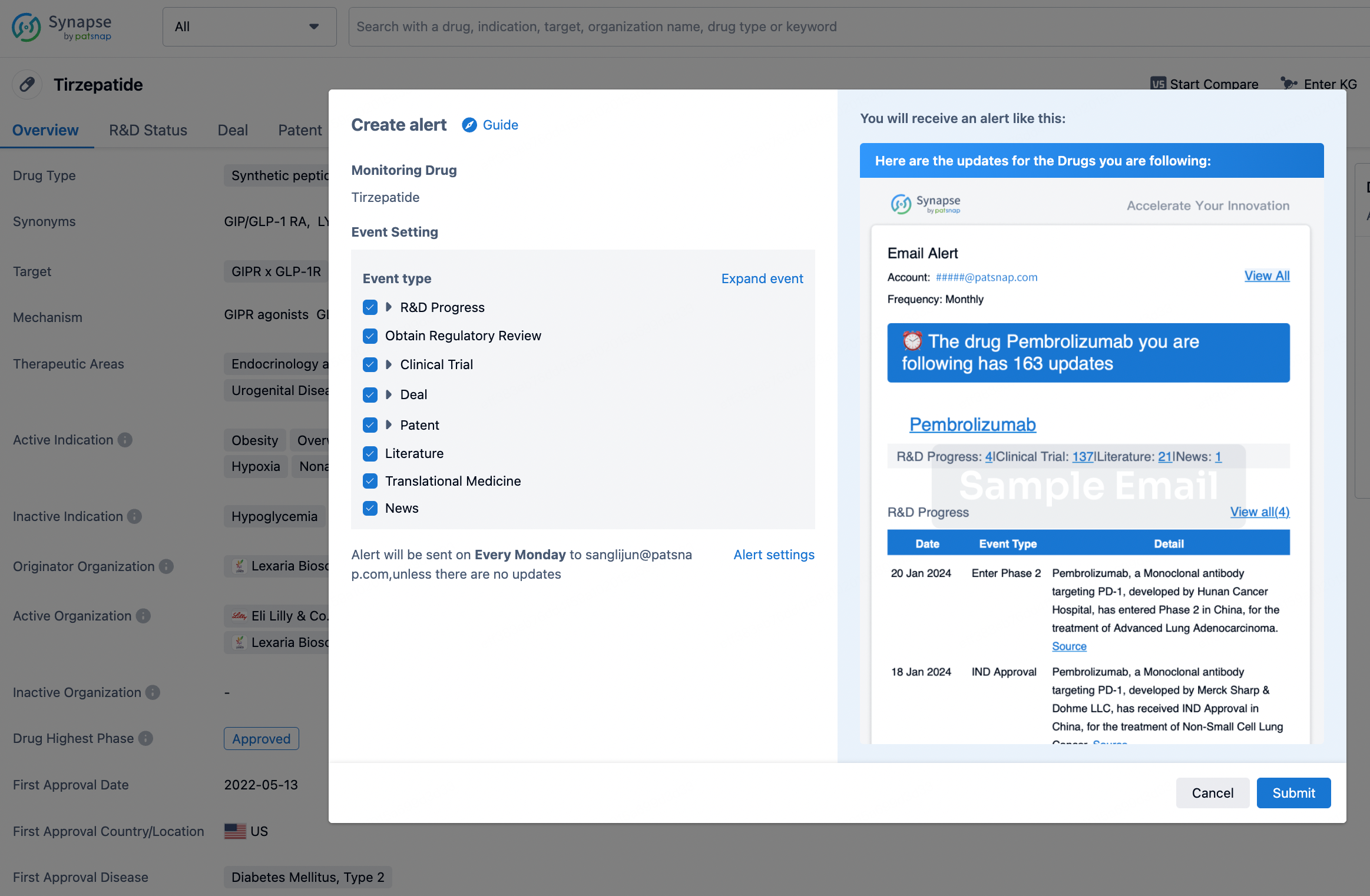
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.