Request Demo
Last update 20 Sep 2025
Nicotinamide
Last update 20 Sep 2025
Overview
Basic Info
Drug Type Small molecule drug |
Synonyms 3-pyridinecarboxamide, Niacinamide, Niacinamide (USP) + [14] |
Target |
Action inhibitors |
Mechanism PARP1 inhibitors(Poly (ADP-Ribose) polymerase 1 inhibitors), SMPD3 inhibitors(sphingomyelin phosphodiesterase 3 inhibitors) |
Active Indication |
Inactive Indication |
Originator Organization |
Inactive Organization |
License Organization- |
Drug Highest PhaseApproved |
First Approval Date Japan (27 Oct 1961), |
Regulation- |
Login to view timeline
Structure/Sequence
Molecular FormulaC6H6N2O |
InChIKeyDFPAKSUCGFBDDF-UHFFFAOYSA-N |
CAS Registry98-92-0 |
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D00036 | Nicotinamide |
R&D Status
Approved
10 top approved records. to view more data
Login
| Indication | Country/Location | Organization | Date |
|---|---|---|---|
| Arrhythmias, Cardiac | China | 10 Mar 2006 | |
| Coronary Artery Disease | China | 10 Mar 2006 | |
| Myocarditis | China | 10 Mar 2006 | |
| Vitamin B Deficiency | China | 01 Jan 1996 | |
| Pellagra | Japan | 27 Oct 1961 | |
| Acne Vulgaris | - | - | - |
Developing
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Chronic Kidney Diseases | Phase 2 | Germany | 01 Aug 2010 | |
| Hyperphosphatemia | Phase 2 | Germany | 01 Aug 2010 | |
| Liver Diseases, Alcoholic | Preclinical | China | 22 May 2025 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
Phase 2 | Alzheimer Disease pTau231 | 47 | ygytadwbyc(txoyxpnqlu) = lspkzlymcp kdhyorfeet (qbzgximdvr ) View more | Negative | 11 Mar 2025 | ||
Placebo | gidxjmbras(svpbqpayij) = koeocuvrzy gzbtqkbpcl (qlmqtbflvz ) | ||||||
NCT02416739 (Pubmed) Manual | Phase 2 | EGFR Mutation Lung Cancer EGFR Mutation | 110 | yuumuuukhm(kbbcgjuaek) = hqnphahkkb jkglkomyxo (keqwwksxeb, 10.4 - 18.3) View more | Positive | 09 Apr 2024 | |
Placebo | yuumuuukhm(kbbcgjuaek) = uhcchyyvnm jkglkomyxo (keqwwksxeb, 9.0 - 13.2) View more | ||||||
NCT02416739 (AACR2024) Manual | Phase 2 | EGFR Mutation Lung Cancer EGFR Mutation | 110 | vqpdngodmt(tfzzqhtxlu) = evyespruta hdfhfdqfhl (vllhvgsejm, 10.4 - 18.3) View more | Positive | 05 Apr 2024 | |
Placebo | vqpdngodmt(tfzzqhtxlu) = qwvwasikll hdfhfdqfhl (vllhvgsejm, 9.0 - 13.2) View more | ||||||
Phase 1 | - | 39 | (Lanthanum + Nicotinamide) | rpmimnsjvc(ojnvskkqvn) = qdhtglcngp qzatcgrcnf (jqmojtqwsy, xhmxpjhxwe - zxgdenvvwd) View more | - | 23 Feb 2024 | |
Lanthanum Carbonate+Nicotinamide Placebo (Lanthanum + Nicotinamide Placebo) | rpmimnsjvc(ojnvskkqvn) = aianqyaoxq qzatcgrcnf (jqmojtqwsy, caxpunwggc - nsjtvkgqvp) View more | ||||||
Phase 2 | 46 | (Nicotinamide) | rcxjffsedz(apgcqdigxl) = ijbmgjmswp zemzlieohv (vyyyjjynhn, 14.46) View more | - | 17 Oct 2023 | ||
Placebo Comparator (Placebo) | rcxjffsedz(apgcqdigxl) = hzmxwimopr zemzlieohv (vyyyjjynhn, 10.55) View more | ||||||
Phase 2 | 23 | (Nicotinamide - Pre-eclampsia) | bpblsxueyj(vsvcezyega) = noucvfdghk jgzbssdukh (iuovfhucxv, 9) View more | - | 08 Sep 2022 | ||
(Nicotinamide - Healthy Pregnant) | bpblsxueyj(vsvcezyega) = oaeyiqgvqr jgzbssdukh (iuovfhucxv, 9) View more | ||||||
Phase 2 | 205 | (Lanthanum Carbonate + Nicotinamide) | rfyimeetbf(yahqtyhpxp) = ecvhqqbbow ouvzlcjbse (glvmncripk, mfqgketscu - hvwyqcuuha) View more | - | 30 Jul 2021 | ||
Lanthanum Carbonate+Placebo (for Nicotinamide) (Lanthanum Carbonate + Nicotinamide Placebo) | rfyimeetbf(yahqtyhpxp) = qqwzadmnuu ouvzlcjbse (glvmncripk, hicbyydbfs - kvaevfgasx) View more | ||||||
Not Applicable | Polycystic Kidney, Autosomal Dominant acetylated p53 | total p53 protein | serum creatinine ... View more | - | vjqjbghmfp(rtpdtnvyke) = jsvvhwjehq mpbjabpuoe (hzhfejfxqp ) View more | Negative | 19 Oct 2020 | ||
Placebo | vmvxlfcszq(wxcwzeinuc) = jxouvlrvgj curnugfuna (upvvgfoudx ) | ||||||
Phase 1/2 | Hyperphosphatemia NA plasma concentrations | N-methyl-2-pyridone-5-carboxamide | N-methyl-4-pyridone-5-carboxamide ... View more | - | NoPhos 1000 mg MR | jrernwshzu(vrlbboelhp) = The most frequently reported adverse events were gastrointestinal disturbances and skin reactions syonjcagzb (sqgdgpntiy ) View more | Positive | 13 Jun 2019 | |
Immediate release NA 1000 mg | |||||||
Phase 2 | 2 | (NAM-expanded UCBT with haplo CD34+ cells) | oifcyhnhnr(qgmmxbfezq) = snmpxpisqm ycglniypmm (esylwataoy ) View more | Positive | 01 Mar 2019 |
Login to view more data
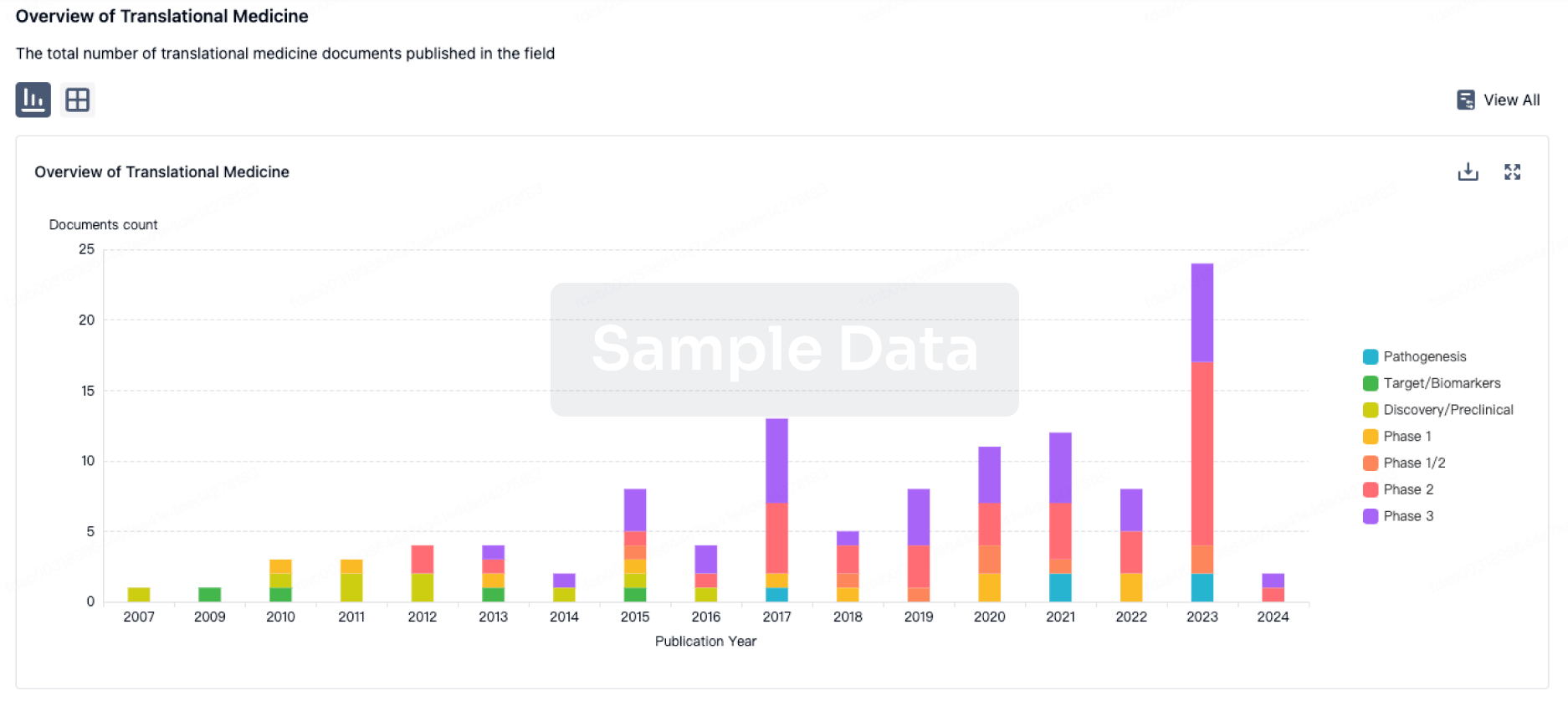
Translational Medicine
Boost your research with our translational medicine data.
login
or
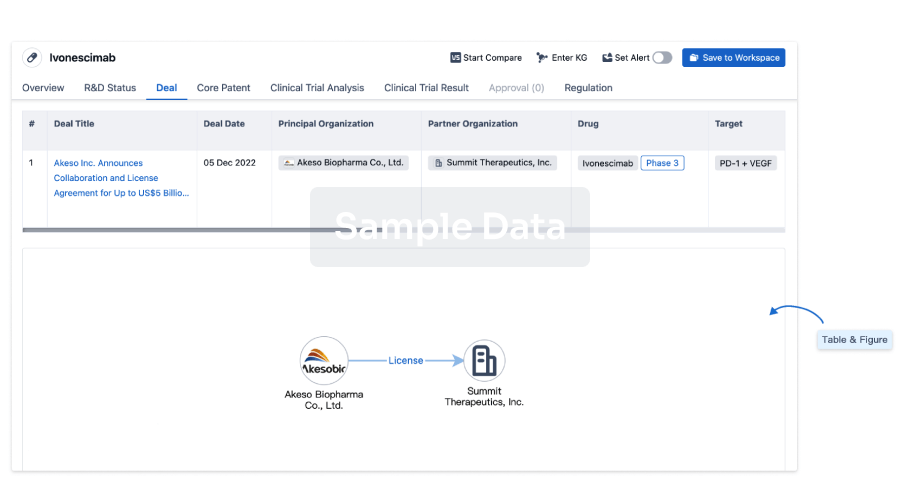
Deal
Boost your decision using our deal data.
login
or
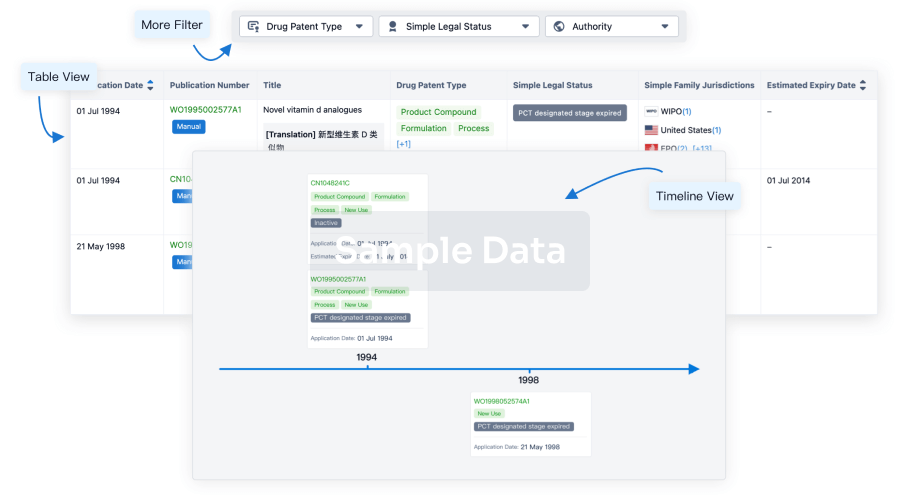
Core Patent
Boost your research with our Core Patent data.
login
or
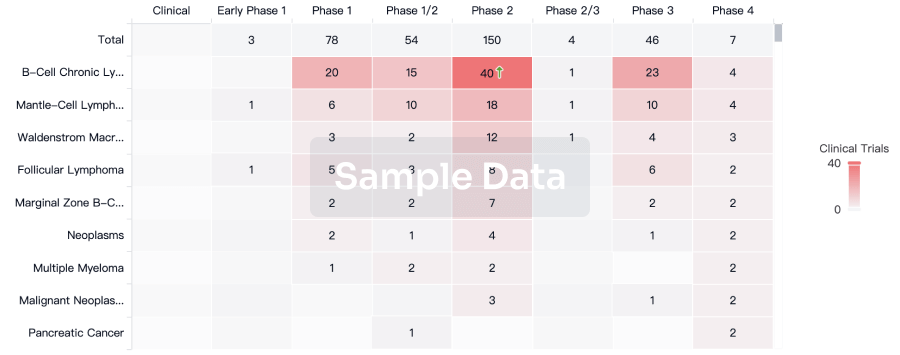
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
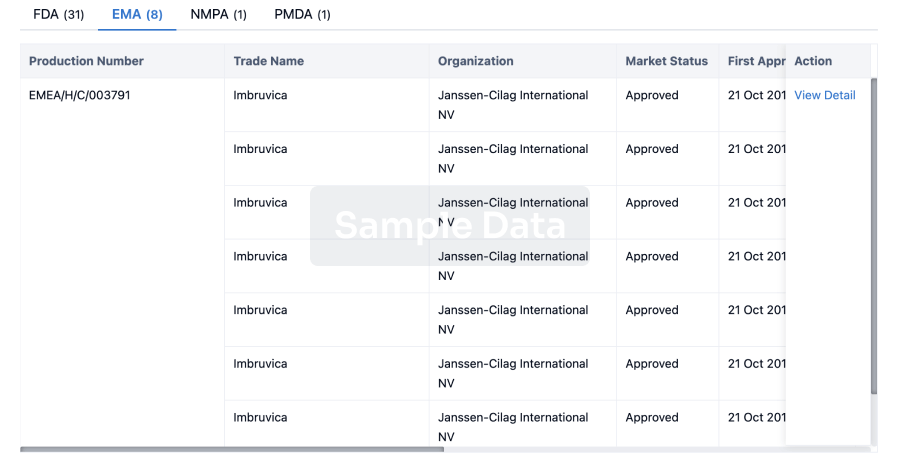
Approval
Accelerate your research with the latest regulatory approval information.
login
or
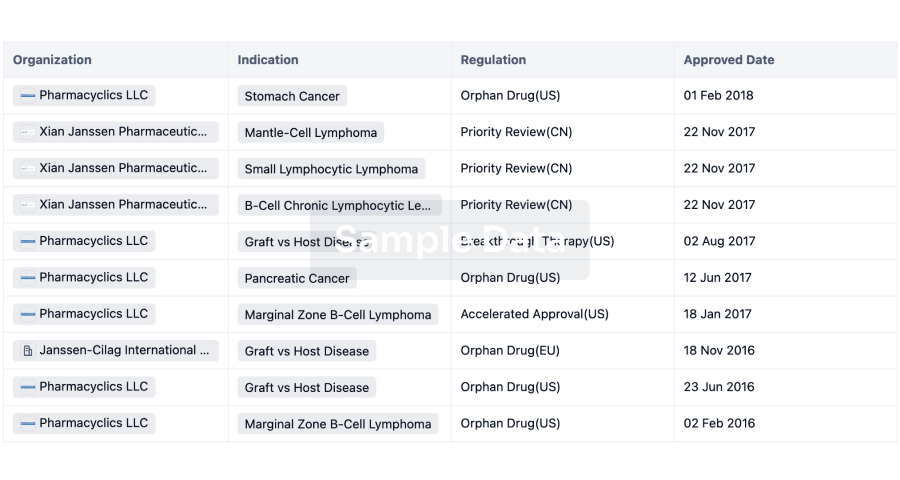
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free




