Request Demo
Last update 08 May 2025
SRC x JAK2
Last update 08 May 2025
Related
4
Drugs associated with SRC x JAK2Target |
Mechanism JAK2 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhasePhase 2 |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism JAK2 inhibitors [+2] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
Target |
Mechanism JAK2 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
1
Clinical Trials associated with SRC x JAK2NCT01423851
A Phase 1/2, Open-label, Dose-Escalation Multi-center Study to Assess the Safety, Tolerability, PK and PD of Orally Administered NS-018 in Patients With Primary Myelofibrosis (MF), Post-polycythemia Vera MF, or Post-essential Thrombocythemia MF
The purpose of this study is to determine the safety and tolerability of orally administered NS-018 in patients with Primary Myelofibrosis (PMF), Post-polycythemia Vera Myelofibrosis (post-PV MF), or Post-essential Thrombocythemia Myelofibrosis (post-ET MF)
Start Date01 Jun 2011 |
Sponsor / Collaborator |
100 Clinical Results associated with SRC x JAK2
Login to view more data
100 Translational Medicine associated with SRC x JAK2
Login to view more data
0 Patents (Medical) associated with SRC x JAK2
Login to view more data
338
Literatures (Medical) associated with SRC x JAK201 Apr 2025·Phytomedicine
Norwogonin attenuates LPS-induced acute lung injury through inhibiting Src/AKT1/NF-κB signaling pathway
Article
Author: Li, An-Qing ; Cao, Tianjiao ; Sun, Kai ; Liu, Jian ; Zhang, Yi ; Han, Jing-Yan ; Wang, Di ; Xie, Ting-Ting ; Yan, Li ; Pan, Chun-Shui ; Weng, Ding-Zhou
01 Apr 2025·Journal of Cellular Biochemistry
The Molecular Mechanisms of Bergapten Against Abdominal Aortic Aneurysm: Evidence From Network Pharmacology, Molecular Docking/Dynamics, and Experimental Validation
Article
Author: Zhong, Lintao ; Huang, Zhenhua ; Li, Tian ; Xu, Fujia ; Si, Xiaoyun ; Luo, Sihan ; Wang, Junfen
24 Mar 2025·Journal of Biomolecular Structure and Dynamics
Lead optimization of
Allium sativum
L. compounds for PTP1B inhibition in diabetes treatment:
in silico
molecular docking and dynamics simulation
Article
Author: Nwobodo, Valentine Osita ; Johnson, Titilayo Omolara ; Adeduro, Mary Nneka ; Taiwo, Odunayo Anthonia ; Adegboyega, Abayomi Emmanuel ; Olowosoke, Christopher Busayo ; Onuh, Kingsley ; Umedum, Ngozi Lillian ; Alemika, Taiwo Emmanuel ; Johnson, Grace Inioluwa ; Elekan, Ayodele O. ; Ojo, Oluwafemi Adeleke
1
News (Medical) associated with SRC x JAK216 Aug 2021
SAN DIEGO, Aug. 16, 2021 (GLOBE NEWSWIRE) -- Turning Point Therapeutics, Inc. (NASDAQ: TPTX), a precision oncology company developing next-generation therapies that target genetic drivers of cancer, today announced initiation of the first cohort of its Phase 1b/2 TRIDENT-2 combination study of lead investigational drug repotrectinib. The initial cohort will investigate repotrectinib in combination with MEK-inhibitor trametinib in KRAS G12D mutated advanced solid tumors.
“We are pleased to initiate the TRIDENT-2 study and explore a potential new treatment option for patients with KRAS-driven solid tumors,” said Mohammad Hirmand, executive vice president and chief medical officer. “With preclinical studies demonstrating repotrectinib’s ability to inhibit JAK2, SRC and FAK, our goal is to help improve the effectiveness of KRAS-targeting agents by suppressing known pathways of tumor resistance.”
The Phase 1b portion of the study will examine the safety, tolerability, pharmacokinetics, and any early signals of efficacy of repotrectinib in combination with trametinib in patients with KRAS G12D mutated advanced solid tumors. After determination of a recommended Phase 2 combination dose, the study includes a Phase 2 dose expansion portion with the primary endpoint of objective response rate.
Results from preclinical studies presented at the 2021 American Association for Cancer Research annual meeting found that repotrectinib in combination with trametinib was more effective than single-agent trametinib in patient-derived KRAS mutant G12D lung cancer models. The repotrectinib-trametinib combination suppressed a broad range of downstream mutant KRAS G12D signaling, increased cell cycle arrest and induction of apoptosis, and was more active in multiple KRAS G12D dependent models compared to either single-agent treatment.
The frequently mutated Kirsten Rat Sarcoma (KRAS) viral oncogene is associated with a broad range of human cancers, including approximately 30% of non-small cell lung, 40% of colorectal and more than 90% of pancreatic cancers. KRAS G12D mutations are known to occur across multiple tumors types, including an estimated 30% of pancreatic, 15% of colorectal and 5% of both endometrial and non-small cell lung cancers.
Therapeutic targeting of KRAS has proven challenging, in part due to resistance and adaptive upregulation of alternative signaling pathways that promote tumor cell survival, as well as concurrent secretion of various cytokines and growth factors.
About Turning Point Therapeutics Inc.Turning Point Therapeutics is a clinical-stage precision oncology company with a pipeline of internally discovered investigational drugs designed to address key limitations of existing cancer therapies. The company’s lead drug candidate, repotrectinib, is a next-generation kinase inhibitor targeting the ROS1 and TRK oncogenic drivers of non-small cell lung cancer and advanced solid tumors. Repotrectinib, which is being studied in a registrational Phase 2 study in adults and a Phase 1/2 study in pediatric patients, has shown antitumor activity and durable responses among kinase inhibitor treatment-naïve and pre-treated patients. The company’s pipeline of drug candidates also includes TPX-0022, targeting MET, CSF1R and SRC, which is being studied in a Phase 1 trial of patients with advanced or metastatic solid tumors harboring genetic alterations in MET; TPX-0046, targeting RET, which is being studied in a Phase 1/2 trial of patients with advanced or metastatic solid tumors harboring genetic alterations in RET; and TPX-0131, a next-generation ALK inhibitor, which is being studied in a Phase 1/2 trial of previously treated patients with ALK-positive advanced or metastatic non-small cell lung cancer. Turning Point’s next-generation kinase inhibitors are designed to bind to their targets with greater precision and affinity than existing therapies, with a novel, compact structure that has demonstrated an ability to potentially overcome treatment resistance common with other kinase inhibitors. The company is driven to develop therapies that mark a turning point for patients in their cancer treatment. For more information, visit .
Forward Looking StatementsStatements contained in this press release regarding matters that are not historical facts are “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995. Such forward-looking statements include statements regarding, among other things, the efficacy, safety and therapeutic potential of repotrectinib, the results, conduct, progress and timing of Turning Point Therapeutics’ pre-clinical studies and clinical trials and plans regarding future clinical trials. Because such statements are subject to risks and uncertainties, actual results may differ materially from those expressed or implied by such forward-looking statements. Words such as “plans”, “will”, “believes,” “anticipates,” “expects,” “intends,” “goal,” “potential” and similar expressions are intended to identify forward-looking statements. These forward-looking statements are based upon Turning Point Therapeutics’ current expectations and involve assumptions that may never materialize or may prove to be incorrect. Actual results could differ materially from those anticipated in such forward-looking statements as a result of various risks and uncertainties, which include, without limitation, risks and uncertainties associated with Turning Point Therapeutics’ business in general, risks and uncertainties related to the impact of the COVID-19 pandemic to Turning Point’s business and the other risks described in Turning Point Therapeutics’ filings with the SEC, including its quarterly report on Form 10-Q filed with the SEC on August 9, 2021. All forward-looking statements contained in this press release speak only as of the date on which they were made. Turning Point Therapeutics undertakes no obligation to update such statements to reflect events that occur or circumstances that exist after the date on which they were made.
AntibodyCollaborateAACR
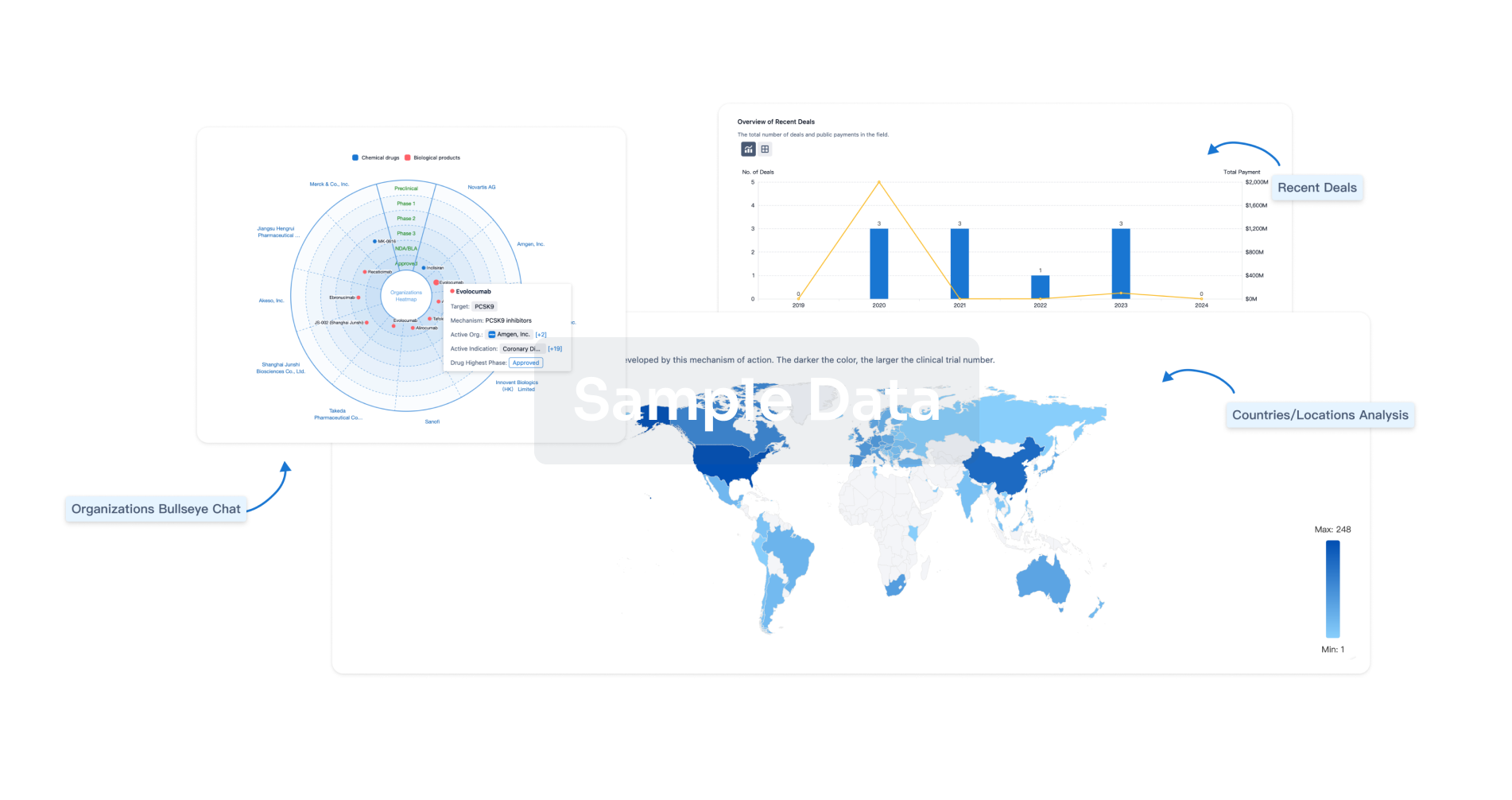
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free



