Request Demo
What is Nasaruplase used for?
14 June 2024
Nasaruplase, a groundbreaking drug in the field of thrombolytic therapy, represents a significant advancement in the treatment of thromboembolic disorders. This recombinant enzyme, often marketed under trade names such as Thrombex and Laseclin, primarily targets the dissolution of blood clots within the vascular system. Developed through collaborative efforts by leading research institutions including the University of Thrombosis Research and the National Cardiovascular Institute, Nasaruplase belongs to the class of drugs known as tissue plasminogen activators (tPAs). Indications for Nasaruplase encompass acute myocardial infarctions, ischemic strokes, and severe pulmonary embolisms. Currently, Nasaruplase is undergoing phase III clinical trials, showing promising results that could revolutionize emergency medical responses to life-threatening clot-related conditions.
The mechanism by which Nasaruplase functions is both intricate and highly effective. As a tissue plasminogen activator, Nasaruplase works by converting plasminogen, a precursor molecule present in the blood, into plasmin, an enzyme responsible for breaking down fibrin clots. Fibrin is the protein that forms the structural framework of a blood clot, and its degradation is essential for dissolving clots that could obstruct blood flow to critical organs. Nasaruplase specifically binds to fibrin within the clot, ensuring localized and efficient clot breakdown while minimizing systemic effects. This targeted mechanism not only enhances the drug's effectiveness but also reduces the risk of widespread bleeding, a common complication associated with earlier thrombolytic therapies.
Administering Nasaruplase requires precision and promptness, often facilitated in a hospital or emergency setting. The drug is typically delivered intravenously, allowing for rapid entry into the bloodstream. The dosage and administration method are carefully tailored to the patient's condition and the severity of the thromboembolic event. For acute myocardial infarction, a rapid bolus injection might be followed by a continuous infusion over several hours to ensure sustained clot dissolution. The onset of action for Nasaruplase is remarkably swift, with clot breakdown commencing within minutes of administration. This rapid response is crucial in emergency scenarios where time is of the essence to restore blood flow and minimize tissue damage.
Like all potent therapeutic agents, Nasaruplase comes with a profile of potential side effects and contraindications that must be meticulously managed. Common side effects include minor bleeding at the injection site, which is generally manageable but requires monitoring. More severe bleeding complications, such as intracranial hemorrhage or gastrointestinal bleeding, though rare, are serious concerns and necessitate immediate medical intervention. Other side effects might include allergic reactions, hypotension, and transient arrhythmias. Contraindications for Nasaruplase use include recent major surgery, active internal bleeding, and a history of hemorrhagic stroke. Patients with severe uncontrolled hypertension or known hypersensitivity to tPAs are also advised against using Nasaruplase. Due to these potential risks, healthcare providers must conduct thorough patient assessments before administration.
The pharmacological interactions of Nasaruplase with other drugs are another critical aspect that requires careful consideration. Anticoagulants, such as warfarin and heparin, can significantly amplify the bleeding risk when used concomitantly with Nasaruplase. As both classes of drugs affect the blood's clotting ability, their combined effects necessitate vigilant monitoring and dosage adjustments. Similarly, antiplatelet agents like aspirin and clopidogrel can interact with Nasaruplase, increasing the likelihood of bleeding complications. It is essential for healthcare providers to review all medications that a patient is taking to prevent adverse interactions. Additionally, nonsteroidal anti-inflammatory drugs (NSAIDs), which are commonly used for pain relief, can further exacerbate bleeding risks when taken alongside Nasaruplase. In emergency settings, where drug histories might be incomplete, healthcare professionals must exercise heightened caution and employ additional hemostatic measures as necessary.
In conclusion, Nasaruplase holds immense promise for the management of thromboembolic conditions, with its targeted mechanism of action, rapid onset, and potential to improve patient outcomes in critical scenarios. However, its use must be carefully balanced against the potential for serious side effects and drug interactions. As research progresses and clinical trials continue to affirm its safety and efficacy, Nasaruplase is poised to become a vital tool in the arsenal of thrombolytic therapies, offering hope and enhanced recovery to patients facing life-threatening blood clots.
The mechanism by which Nasaruplase functions is both intricate and highly effective. As a tissue plasminogen activator, Nasaruplase works by converting plasminogen, a precursor molecule present in the blood, into plasmin, an enzyme responsible for breaking down fibrin clots. Fibrin is the protein that forms the structural framework of a blood clot, and its degradation is essential for dissolving clots that could obstruct blood flow to critical organs. Nasaruplase specifically binds to fibrin within the clot, ensuring localized and efficient clot breakdown while minimizing systemic effects. This targeted mechanism not only enhances the drug's effectiveness but also reduces the risk of widespread bleeding, a common complication associated with earlier thrombolytic therapies.
Administering Nasaruplase requires precision and promptness, often facilitated in a hospital or emergency setting. The drug is typically delivered intravenously, allowing for rapid entry into the bloodstream. The dosage and administration method are carefully tailored to the patient's condition and the severity of the thromboembolic event. For acute myocardial infarction, a rapid bolus injection might be followed by a continuous infusion over several hours to ensure sustained clot dissolution. The onset of action for Nasaruplase is remarkably swift, with clot breakdown commencing within minutes of administration. This rapid response is crucial in emergency scenarios where time is of the essence to restore blood flow and minimize tissue damage.
Like all potent therapeutic agents, Nasaruplase comes with a profile of potential side effects and contraindications that must be meticulously managed. Common side effects include minor bleeding at the injection site, which is generally manageable but requires monitoring. More severe bleeding complications, such as intracranial hemorrhage or gastrointestinal bleeding, though rare, are serious concerns and necessitate immediate medical intervention. Other side effects might include allergic reactions, hypotension, and transient arrhythmias. Contraindications for Nasaruplase use include recent major surgery, active internal bleeding, and a history of hemorrhagic stroke. Patients with severe uncontrolled hypertension or known hypersensitivity to tPAs are also advised against using Nasaruplase. Due to these potential risks, healthcare providers must conduct thorough patient assessments before administration.
The pharmacological interactions of Nasaruplase with other drugs are another critical aspect that requires careful consideration. Anticoagulants, such as warfarin and heparin, can significantly amplify the bleeding risk when used concomitantly with Nasaruplase. As both classes of drugs affect the blood's clotting ability, their combined effects necessitate vigilant monitoring and dosage adjustments. Similarly, antiplatelet agents like aspirin and clopidogrel can interact with Nasaruplase, increasing the likelihood of bleeding complications. It is essential for healthcare providers to review all medications that a patient is taking to prevent adverse interactions. Additionally, nonsteroidal anti-inflammatory drugs (NSAIDs), which are commonly used for pain relief, can further exacerbate bleeding risks when taken alongside Nasaruplase. In emergency settings, where drug histories might be incomplete, healthcare professionals must exercise heightened caution and employ additional hemostatic measures as necessary.
In conclusion, Nasaruplase holds immense promise for the management of thromboembolic conditions, with its targeted mechanism of action, rapid onset, and potential to improve patient outcomes in critical scenarios. However, its use must be carefully balanced against the potential for serious side effects and drug interactions. As research progresses and clinical trials continue to affirm its safety and efficacy, Nasaruplase is poised to become a vital tool in the arsenal of thrombolytic therapies, offering hope and enhanced recovery to patients facing life-threatening blood clots.
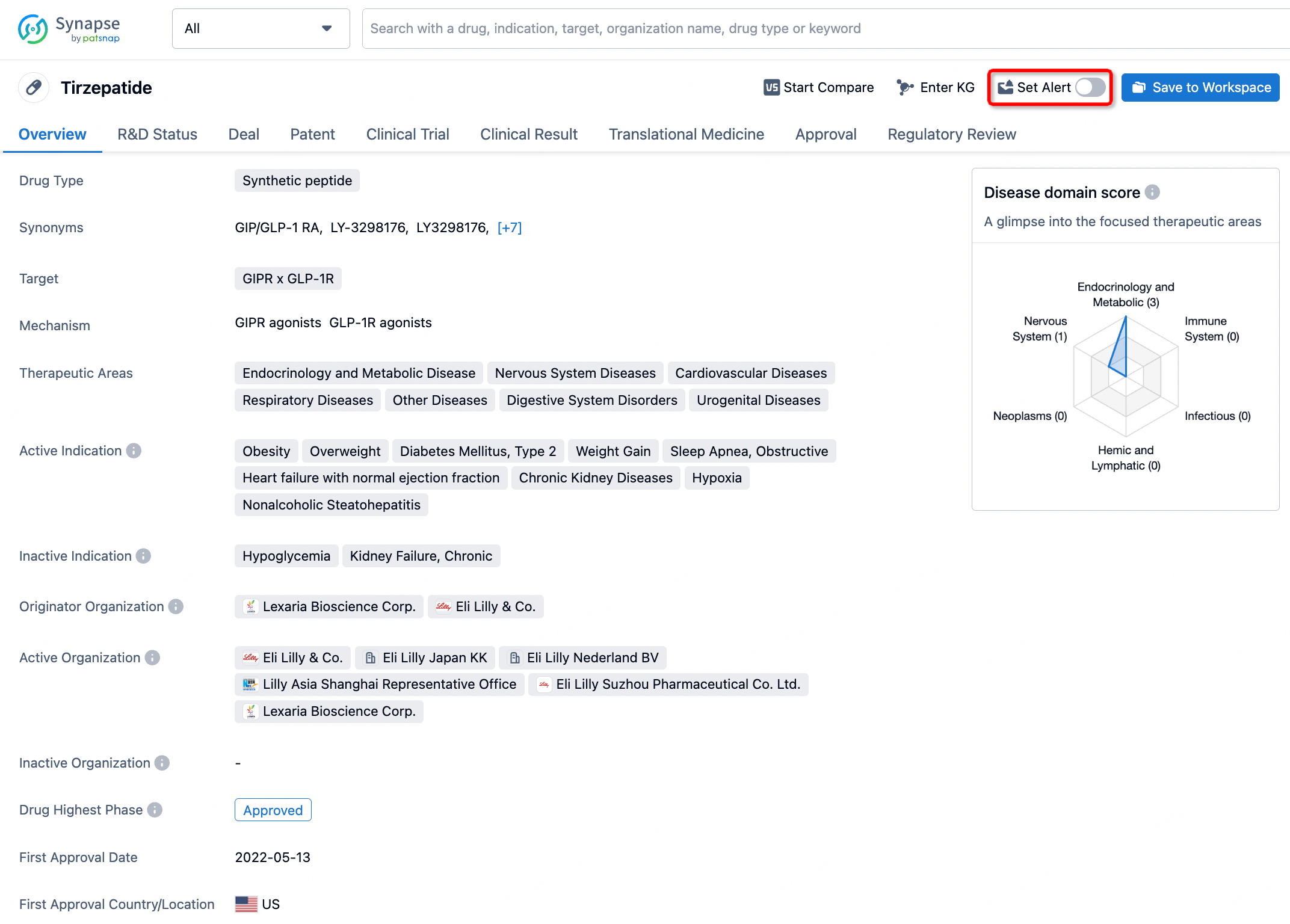
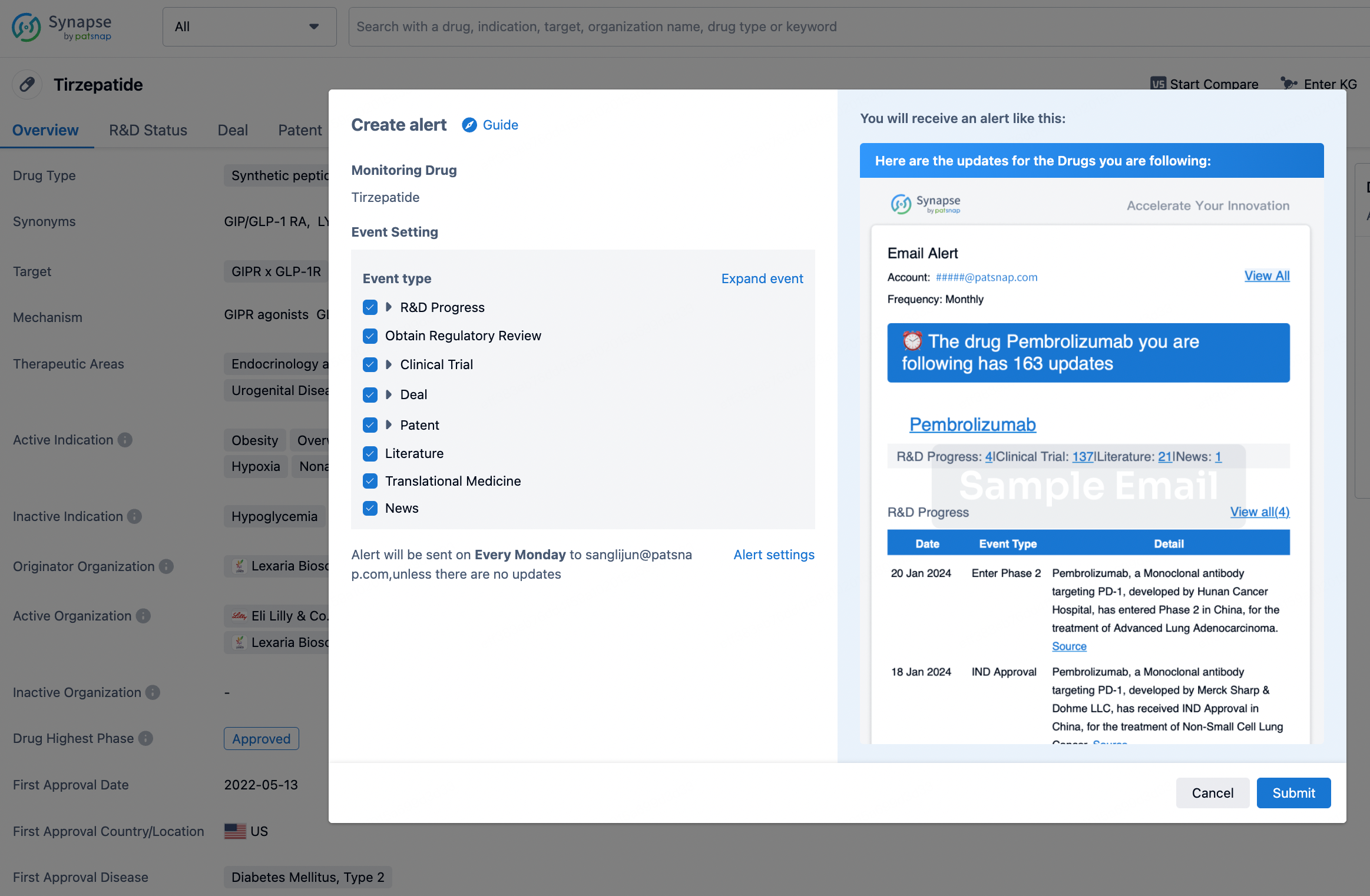
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.