Request Demo
What are AC inhibitors and how do they work?
25 June 2024
Angiotensin-converting enzyme (ACE) inhibitors are a class of medications that are commonly prescribed to treat a variety of cardiovascular and renal conditions. These drugs have significantly impacted the management of hypertension and heart failure, contributing to improved patient outcomes. Understanding the function, mechanism of action, and clinical applications of ACE inhibitors can help patients and healthcare providers make informed decisions about their use.
Introduction to ACE Inhibitors
ACE inhibitors are widely recognized for their role in the treatment of high blood pressure (hypertension) and heart failure. These medications were first discovered in the 1970s and have since become a cornerstone of cardiovascular therapy. They are named for their primary mechanism of action: the inhibition of the angiotensin-converting enzyme. By blocking this enzyme, ACE inhibitors can reduce blood pressure, decrease strain on the heart, and improve overall cardiovascular health. Some common ACE inhibitors include enalapril, lisinopril, and ramipril, among others.
How Do ACE Inhibitors Work?
To understand how ACE inhibitors work, it's crucial to grasp the basics of the renin-angiotensin-aldosterone system (RAAS), a hormone system that regulates blood pressure and fluid balance. When blood pressure is low, the kidneys release an enzyme called renin. Renin then converts angiotensinogen, a protein produced by the liver, into angiotensin I. This is where the angiotensin-converting enzyme (ACE) comes into play: it converts angiotensin I into angiotensin II, a potent vasoconstrictor that narrows blood vessels and increases blood pressure. Angiotensin II also stimulates the release of aldosterone from the adrenal glands, promoting sodium and water retention, which further raises blood pressure.
ACE inhibitors interrupt this process by blocking the conversion of angiotensin I to angiotensin II. As a result, blood vessels relax and dilate, leading to a reduction in blood pressure. Additionally, the decreased levels of angiotensin II mean less aldosterone release, which helps reduce sodium and water retention. This dual action makes ACE inhibitors particularly effective in managing conditions where lowering blood pressure and reducing fluid overload are essential.
What Are ACE Inhibitors Used For?
ACE inhibitors are primarily used to treat hypertension, one of the most common chronic conditions worldwide. High blood pressure is a significant risk factor for heart disease, stroke, and kidney disease. By lowering blood pressure, ACE inhibitors help reduce these risks. They are often prescribed as a first-line treatment or in combination with other antihypertensive medications, such as diuretics or calcium channel blockers.
Heart failure is another major indication for ACE inhibitors. Heart failure occurs when the heart cannot pump blood effectively, leading to symptoms like shortness of breath, fatigue, and fluid retention. ACE inhibitors help alleviate these symptoms by reducing the workload on the heart and preventing fluid buildup. Clinical studies have shown that ACE inhibitors can improve survival rates and quality of life in patients with heart failure.
Beyond hypertension and heart failure, ACE inhibitors are also used in the management of chronic kidney disease (CKD), particularly in patients with diabetes. High blood pressure and diabetes can both damage the kidneys over time, leading to CKD. By lowering blood pressure and reducing proteinuria (the presence of excess protein in the urine), ACE inhibitors can slow the progression of kidney damage.
In some cases, ACE inhibitors are prescribed after a heart attack (myocardial infarction) to improve survival rates and reduce the likelihood of future cardiac events. They achieve this by lowering blood pressure, reducing the workload on the heart, and preventing harmful remodeling of heart tissue that can occur after a heart attack.
In summary, ACE inhibitors are a versatile and effective class of medications widely used in the treatment of hypertension, heart failure, chronic kidney disease, and post-myocardial infarction care. Their ability to interfere with the RAAS makes them uniquely suited to managing conditions where blood pressure control and fluid balance are critical. As always, it's essential for patients to consult with their healthcare providers to determine the most appropriate treatment plan for their specific needs.
Introduction to ACE Inhibitors
ACE inhibitors are widely recognized for their role in the treatment of high blood pressure (hypertension) and heart failure. These medications were first discovered in the 1970s and have since become a cornerstone of cardiovascular therapy. They are named for their primary mechanism of action: the inhibition of the angiotensin-converting enzyme. By blocking this enzyme, ACE inhibitors can reduce blood pressure, decrease strain on the heart, and improve overall cardiovascular health. Some common ACE inhibitors include enalapril, lisinopril, and ramipril, among others.
How Do ACE Inhibitors Work?
To understand how ACE inhibitors work, it's crucial to grasp the basics of the renin-angiotensin-aldosterone system (RAAS), a hormone system that regulates blood pressure and fluid balance. When blood pressure is low, the kidneys release an enzyme called renin. Renin then converts angiotensinogen, a protein produced by the liver, into angiotensin I. This is where the angiotensin-converting enzyme (ACE) comes into play: it converts angiotensin I into angiotensin II, a potent vasoconstrictor that narrows blood vessels and increases blood pressure. Angiotensin II also stimulates the release of aldosterone from the adrenal glands, promoting sodium and water retention, which further raises blood pressure.
ACE inhibitors interrupt this process by blocking the conversion of angiotensin I to angiotensin II. As a result, blood vessels relax and dilate, leading to a reduction in blood pressure. Additionally, the decreased levels of angiotensin II mean less aldosterone release, which helps reduce sodium and water retention. This dual action makes ACE inhibitors particularly effective in managing conditions where lowering blood pressure and reducing fluid overload are essential.
What Are ACE Inhibitors Used For?
ACE inhibitors are primarily used to treat hypertension, one of the most common chronic conditions worldwide. High blood pressure is a significant risk factor for heart disease, stroke, and kidney disease. By lowering blood pressure, ACE inhibitors help reduce these risks. They are often prescribed as a first-line treatment or in combination with other antihypertensive medications, such as diuretics or calcium channel blockers.
Heart failure is another major indication for ACE inhibitors. Heart failure occurs when the heart cannot pump blood effectively, leading to symptoms like shortness of breath, fatigue, and fluid retention. ACE inhibitors help alleviate these symptoms by reducing the workload on the heart and preventing fluid buildup. Clinical studies have shown that ACE inhibitors can improve survival rates and quality of life in patients with heart failure.
Beyond hypertension and heart failure, ACE inhibitors are also used in the management of chronic kidney disease (CKD), particularly in patients with diabetes. High blood pressure and diabetes can both damage the kidneys over time, leading to CKD. By lowering blood pressure and reducing proteinuria (the presence of excess protein in the urine), ACE inhibitors can slow the progression of kidney damage.
In some cases, ACE inhibitors are prescribed after a heart attack (myocardial infarction) to improve survival rates and reduce the likelihood of future cardiac events. They achieve this by lowering blood pressure, reducing the workload on the heart, and preventing harmful remodeling of heart tissue that can occur after a heart attack.
In summary, ACE inhibitors are a versatile and effective class of medications widely used in the treatment of hypertension, heart failure, chronic kidney disease, and post-myocardial infarction care. Their ability to interfere with the RAAS makes them uniquely suited to managing conditions where blood pressure control and fluid balance are critical. As always, it's essential for patients to consult with their healthcare providers to determine the most appropriate treatment plan for their specific needs.
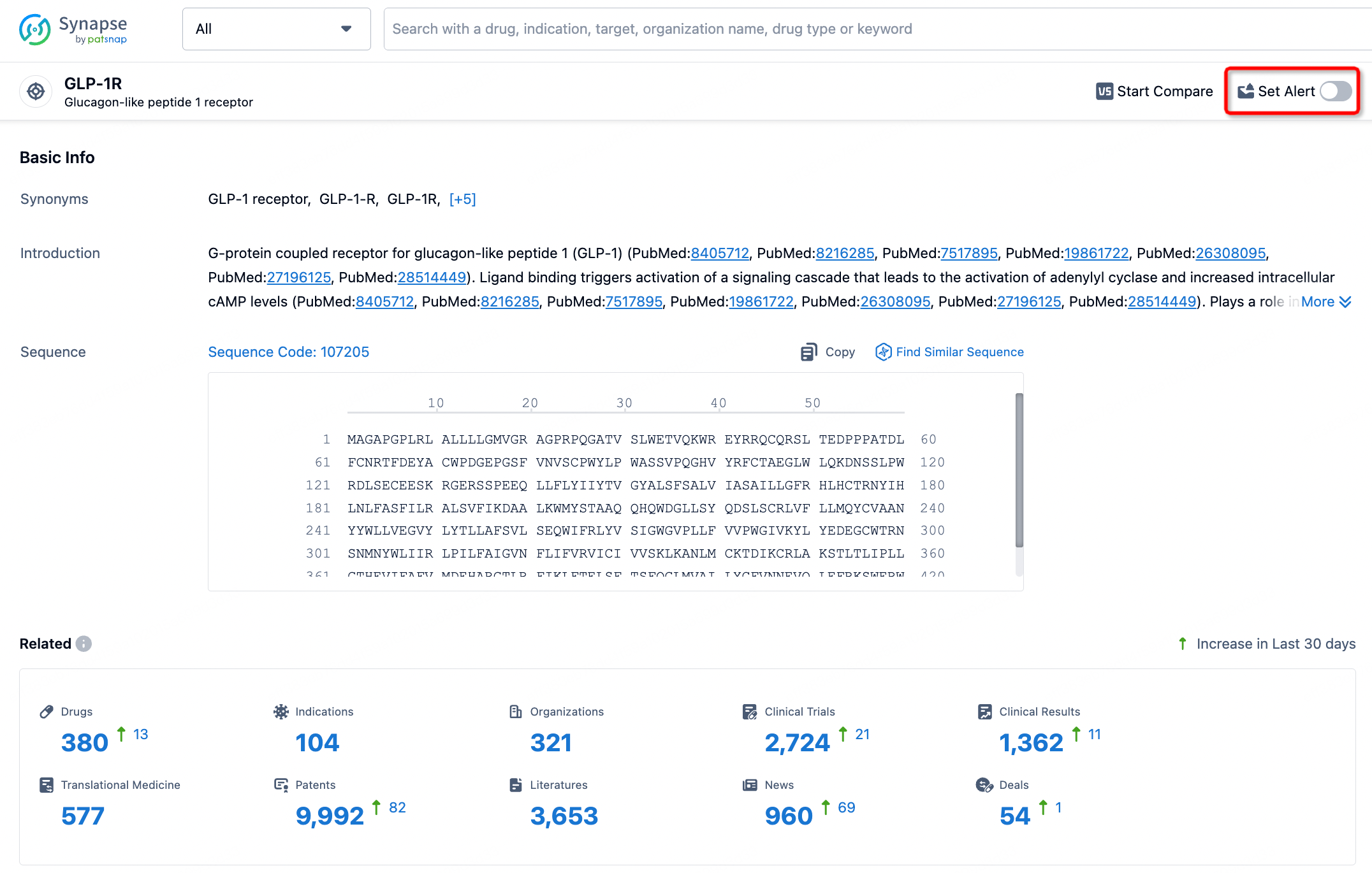
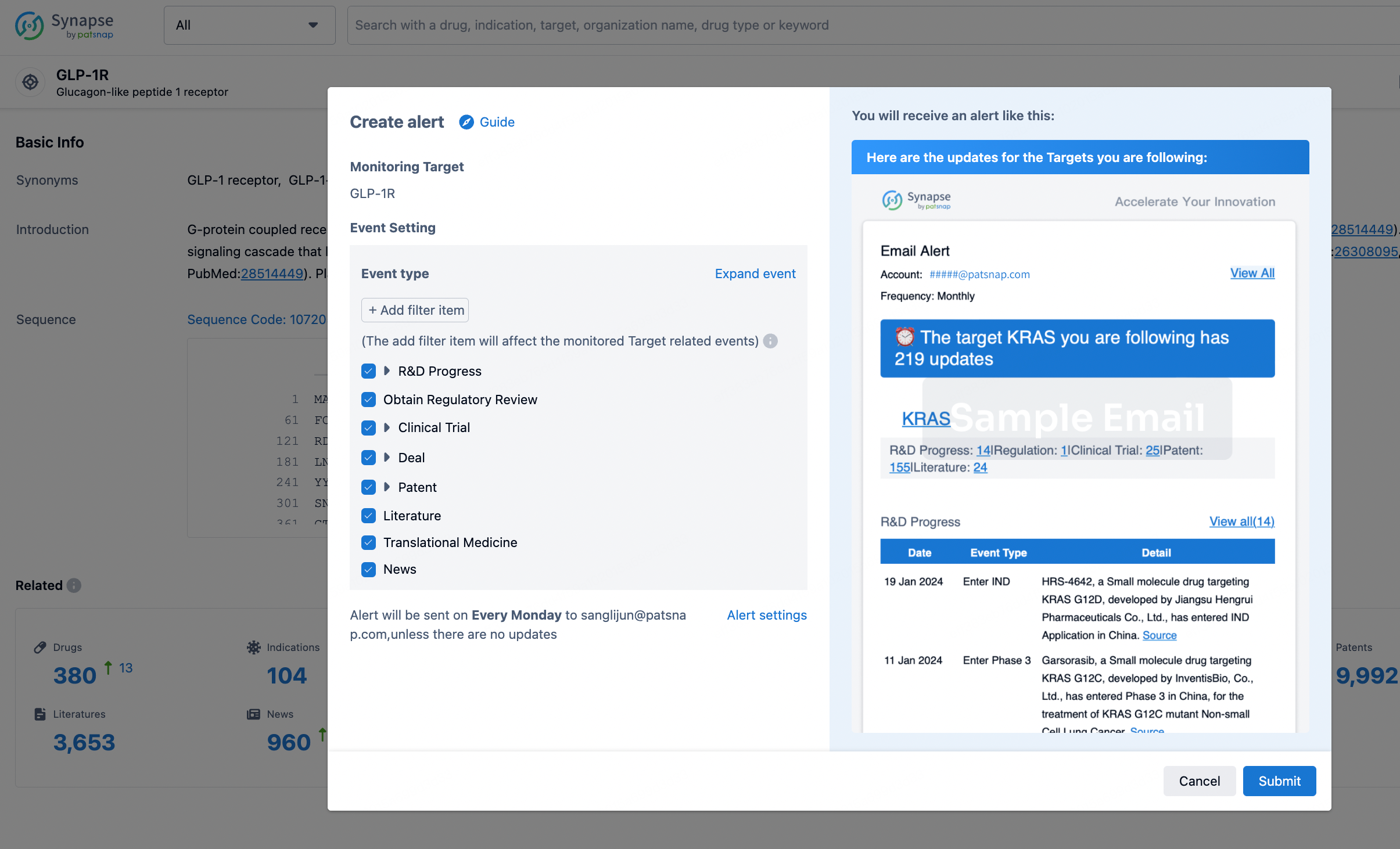
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.