Request Demo
What is Carfilzomib used for?
14 June 2024
Carfilzomib, marketed under the trade name Kyprolis, is a cutting-edge medication designed to treat multiple myeloma, a type of blood cancer that affects plasma cells in the bone marrow. This drug was developed by Onyx Pharmaceuticals, now a subsidiary of Amgen Inc., and has been a game-changer in the realm of oncology since its approval by the U.S. Food and Drug Administration (FDA) in 2012. Carfilzomib is a second-generation proteasome inhibitor, specifically targeting the chymotrypsin-like activity of the 20S proteasome, an essential protein complex involved in degrading unneeded or damaged proteins. By disrupting this process, Carfilzomib induces apoptosis (programmed cell death) in cancer cells, thereby slowing the progression of the disease. The drug is typically administered in combination with other medications like dexamethasone or lenalidomide, enhancing its efficacy in treating relapsed or refractory multiple myeloma. Ongoing research continues to explore additional therapeutic applications and optimize combination regimens to extend the benefits of Carfilzomib to a broader range of patients.
Carfilzomib exerts its therapeutic effects primarily through the irreversible inhibition of the 20S proteasome, a core component of the proteasome complex responsible for protein degradation in cells. This inhibition leads to the accumulation of misfolded and damaged proteins within the cell, inducing a stress response that ultimately triggers apoptosis. Unlike its predecessor, bortezomib, which is a reversible inhibitor, Carfilzomib binds covalently and irreversibly to its target, resulting in prolonged proteasome inhibition and enhanced anti-tumor activity. This unique mechanism of action not only makes Carfilzomib highly effective but also helps overcome resistance mechanisms that some cancer cells develop against first-generation proteasome inhibitors. Moreover, Carfilzomib specifically targets the chymotrypsin-like activity of the proteasome, sparing other proteolytic activities and thereby reducing off-target effects and enhancing its safety profile.
Carfilzomib is administered intravenously, typically through an infusion that lasts around 10 minutes. The drug is usually given two consecutive days per week, for three weeks, followed by a week off, in 28-day cycles. The dosing regimen often starts at a lower dose and may be escalated based on the patient's tolerance and response to the treatment. Before the infusion, patients are pre-medicated with dexamethasone to reduce the risk of infusion-related reactions and other side effects. The onset of Carfilzomib’s action can be quite rapid, with some patients experiencing a response within a few weeks of starting the treatment. However, the full therapeutic benefits may take several cycles to become apparent. It’s crucial for patients to adhere strictly to their dosing schedule and follow their healthcare provider’s instructions to maximize the drug's efficacy and manage potential side effects.
Like all medications, Carfilzomib comes with a range of potential side effects, some of which can be severe. Common side effects include fatigue, nausea, diarrhea, fever, and shortness of breath. More serious adverse effects can also occur, such as cardiac complications (including heart failure and ischemia), hypertension, thrombocytopenia (low platelet count), hepatotoxicity (liver damage), and nephrotoxicity (kidney damage). Due to these potential risks, Carfilzomib is contraindicated in patients with certain pre-existing conditions, such as severe cardiac or pulmonary impairments. It is also not recommended for use during pregnancy, as it can cause harm to the developing fetus. Patients undergoing Carfilzomib therapy require regular monitoring through blood tests and clinical evaluations to detect and manage any adverse effects promptly. Healthcare providers may adjust the dosage or discontinue treatment based on the patient's tolerance and response to the drug.
Several drugs and substances can interact with Carfilzomib, potentially altering its effectiveness or increasing the risk of adverse effects. For instance, concurrent use of strong CYP3A4 inhibitors (such as ketoconazole, ritonavir, or clarithromycin) can elevate Carfilzomib levels in the blood, enhancing its toxic effects. Similarly, CYP3A4 inducers (like rifampin, phenytoin, or St. John’s Wort) can reduce Carfilzomib efficacy by decreasing its plasma concentration. Other medications that affect the cardiovascular system, such as antihypertensives, anticoagulants, and certain anti-arrhythmic drugs, should be used with caution, as they may exacerbate Carfilzomib’s cardiotoxic effects. Patients are advised to inform their healthcare providers about all the medications, supplements, and herbal products they are taking to avoid potential drug interactions. Regular communication between patients and healthcare providers is essential to ensure the safe and effective use of Carfilzomib in the treatment of multiple myeloma.
Carfilzomib exerts its therapeutic effects primarily through the irreversible inhibition of the 20S proteasome, a core component of the proteasome complex responsible for protein degradation in cells. This inhibition leads to the accumulation of misfolded and damaged proteins within the cell, inducing a stress response that ultimately triggers apoptosis. Unlike its predecessor, bortezomib, which is a reversible inhibitor, Carfilzomib binds covalently and irreversibly to its target, resulting in prolonged proteasome inhibition and enhanced anti-tumor activity. This unique mechanism of action not only makes Carfilzomib highly effective but also helps overcome resistance mechanisms that some cancer cells develop against first-generation proteasome inhibitors. Moreover, Carfilzomib specifically targets the chymotrypsin-like activity of the proteasome, sparing other proteolytic activities and thereby reducing off-target effects and enhancing its safety profile.
Carfilzomib is administered intravenously, typically through an infusion that lasts around 10 minutes. The drug is usually given two consecutive days per week, for three weeks, followed by a week off, in 28-day cycles. The dosing regimen often starts at a lower dose and may be escalated based on the patient's tolerance and response to the treatment. Before the infusion, patients are pre-medicated with dexamethasone to reduce the risk of infusion-related reactions and other side effects. The onset of Carfilzomib’s action can be quite rapid, with some patients experiencing a response within a few weeks of starting the treatment. However, the full therapeutic benefits may take several cycles to become apparent. It’s crucial for patients to adhere strictly to their dosing schedule and follow their healthcare provider’s instructions to maximize the drug's efficacy and manage potential side effects.
Like all medications, Carfilzomib comes with a range of potential side effects, some of which can be severe. Common side effects include fatigue, nausea, diarrhea, fever, and shortness of breath. More serious adverse effects can also occur, such as cardiac complications (including heart failure and ischemia), hypertension, thrombocytopenia (low platelet count), hepatotoxicity (liver damage), and nephrotoxicity (kidney damage). Due to these potential risks, Carfilzomib is contraindicated in patients with certain pre-existing conditions, such as severe cardiac or pulmonary impairments. It is also not recommended for use during pregnancy, as it can cause harm to the developing fetus. Patients undergoing Carfilzomib therapy require regular monitoring through blood tests and clinical evaluations to detect and manage any adverse effects promptly. Healthcare providers may adjust the dosage or discontinue treatment based on the patient's tolerance and response to the drug.
Several drugs and substances can interact with Carfilzomib, potentially altering its effectiveness or increasing the risk of adverse effects. For instance, concurrent use of strong CYP3A4 inhibitors (such as ketoconazole, ritonavir, or clarithromycin) can elevate Carfilzomib levels in the blood, enhancing its toxic effects. Similarly, CYP3A4 inducers (like rifampin, phenytoin, or St. John’s Wort) can reduce Carfilzomib efficacy by decreasing its plasma concentration. Other medications that affect the cardiovascular system, such as antihypertensives, anticoagulants, and certain anti-arrhythmic drugs, should be used with caution, as they may exacerbate Carfilzomib’s cardiotoxic effects. Patients are advised to inform their healthcare providers about all the medications, supplements, and herbal products they are taking to avoid potential drug interactions. Regular communication between patients and healthcare providers is essential to ensure the safe and effective use of Carfilzomib in the treatment of multiple myeloma.
How to obtain the latest development progress of all drugs?
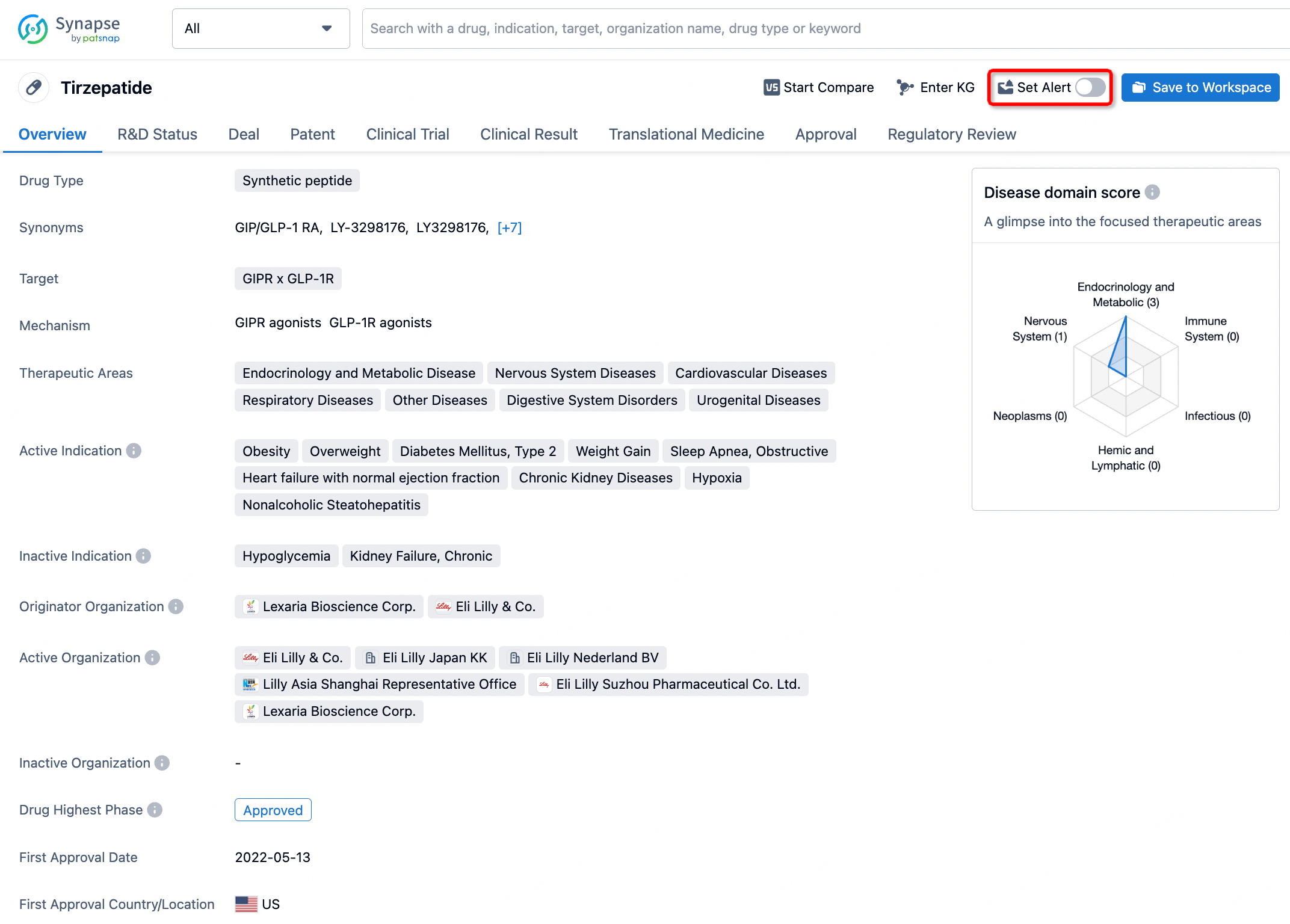
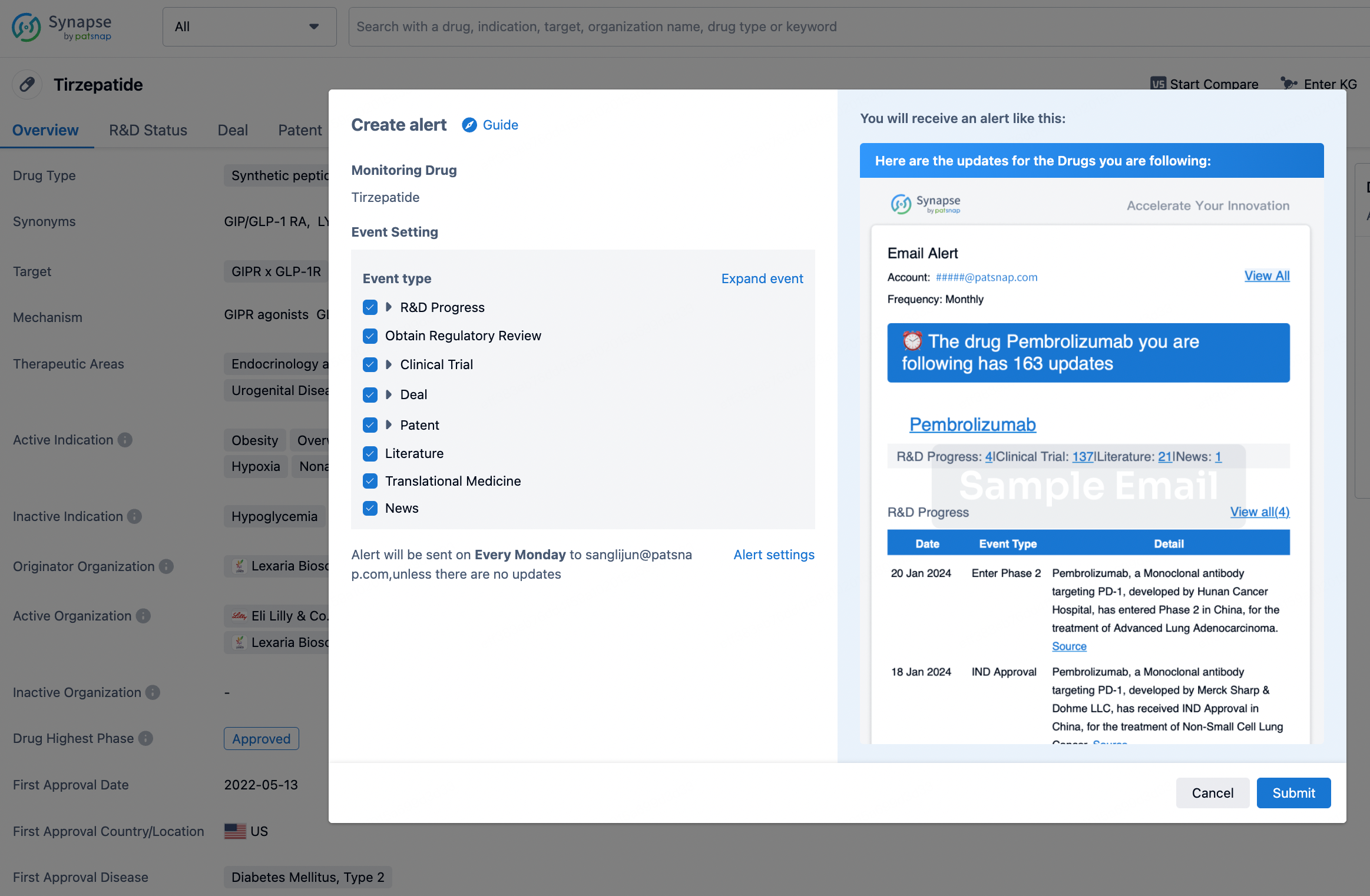
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.