Request Demo
What is Cortisol succinate used for?
15 June 2024
Cortisol succinate, also known by its trade names such as Solu-Cortef and Hydrocortisone sodium succinate, is a synthetic glucocorticoid used predominantly in clinical settings. This medication is developed and researched by numerous pharmaceutical companies and institutions. As a type of corticosteroid, it is designed to mimic the effects of naturally occurring cortisol in the body, which is produced by the adrenal glands. It is primarily indicated for the treatment of conditions that involve inflammation, such as severe allergies, asthma, and arthritis, as well as certain adrenal insufficiencies. Research in recent years has also explored its efficacy in treating septic shock and other critical illnesses, with some promising results. However, its use remains circumscribed by its potential side effects and the need for careful administration and monitoring.
Cortisol succinate Mechanism of Action
The mechanism of action of cortisol succinate involves its role as a synthetic analog of cortisol, a hormone produced by the adrenal cortex. Cortisol plays a vital role in various physiological processes, including the regulation of metabolism, immune response, and stress responses. When administered, cortisol succinate binds to glucocorticoid receptors in the cytoplasm of target cells. This binding initiates a cascade of events that lead to the modulation of gene expression. Specifically, cortisol succinate influences the transcription of anti-inflammatory proteins and the repression of pro-inflammatory genes. This dual action contributes to its potent anti-inflammatory and immunosuppressive properties. Additionally, cortisol succinate stabilizes cell membranes and lysosomal membranes, reducing the release of inflammatory mediators. It also promotes gluconeogenesis, enhances the breakdown of lipids, and influences the distribution of white blood cells, which collectively contribute to its broad-spectrum therapeutic effects.
How to Use Cortisol succinate
Cortisol succinate can be administered through various routes depending on the clinical scenario. The most common methods include intravenous (IV) and intramuscular (IM) injections. The choice of administration depends on the urgency and severity of the condition being treated. Intravenous administration is generally preferred in emergency situations, such as severe asthma attacks or adrenal crisis, due to its rapid onset of action, typically within minutes. Intramuscular injections, on the other hand, provide a more sustained release of the drug and are useful in situations where immediate onset is not as critical.
The dosage of cortisol succinate varies widely based on the condition being treated, the patient's age, and their overall health status. For instance, in the management of acute asthma exacerbations, adult dosages may range from 100 mg to 500 mg administered intravenously every 2 to 6 hours, whereas for adrenal insufficiency, a typical regimen might involve lower dosages given at regular intervals. It is crucial for healthcare providers to individualize the dosing and administration schedule to optimize therapeutic outcomes while minimizing potential side effects.
Patients receiving cortisol succinate should be monitored closely for their response to therapy, and adjustments may be necessary based on clinical feedback. Tapering the dose gradually is often recommended when discontinuing the drug to avoid adrenal insufficiency resulting from sudden withdrawal.
What is Cortisol succinate Side Effects
While cortisol succinate is highly effective in managing a range of inflammatory and autoimmune conditions, its use is not without potential side effects. The side effects can be categorized into short-term and long-term effects.
Short-term side effects may include elevated blood sugar levels, fluid retention, high blood pressure, and mood changes such as irritability or euphoria. Gastrointestinal disturbances, such as nausea and vomiting, may also occur. In some cases, patients may experience a condition known as "steroid-induced psychosis," characterized by changes in mental status, including confusion, hallucinations, and severe mood swings.
Long-term use of cortisol succinate carries a risk of more serious side effects. These include osteoporosis, muscle wasting, and increased susceptibility to infections due to immunosuppression. Prolonged treatment can also lead to the development of Cushing's syndrome, characterized by a round face, central obesity, and skin changes such as striae and bruising. Additionally, chronic use can result in adrenal suppression, where the body's natural cortisol production is inhibited, making it challenging to respond to stress.
Contraindications for the use of cortisol succinate include systemic fungal infections and known hypersensitivity to the drug. Caution is advised in patients with conditions such as diabetes, hypertension, peptic ulcer disease, and psychiatric disorders, as cortisol succinate can exacerbate these conditions. Pregnant and breastfeeding women should use the drug only when clearly needed, as it can cross the placenta and be excreted in breast milk.
What Other Drugs Will Affect Cortisol succinate
The efficacy and safety of cortisol succinate can be influenced by concomitant use of other drugs. Drug interactions can either potentiate its effects, increasing the risk of side effects, or diminish its therapeutic efficacy.
Drugs that induce hepatic enzymes, such as phenytoin, phenobarbital, and rifampin, can increase the metabolism of cortisol succinate, potentially reducing its effectiveness. On the other hand, drugs that inhibit hepatic enzymes, such as ketoconazole and certain antibiotics like erythromycin, can decrease the metabolism of cortisol succinate, increasing the risk of toxicity.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, when used concurrently with cortisol succinate, can increase the risk of gastrointestinal bleeding and ulceration. This combination should be used with caution, and protective measures such as the use of proton pump inhibitors may be considered.
Additionally, diuretics, particularly thiazides and loop diuretics, can exacerbate the hypokalemic effects of cortisol succinate, leading to significant potassium depletion. Patients on such regimens should have their electrolyte levels monitored closely.
Vaccines may also interact with cortisol succinate. Live vaccines, in particular, should be avoided in patients receiving immunosuppressive doses of the drug, as their immune response may be inadequate, and there is a risk of disseminated infection.
In summary, while cortisol succinate is a powerful and versatile drug in the management of various inflammatory and autoimmune conditions, its use requires careful consideration of potential side effects and drug interactions. Close monitoring and individualized dosing are essential to maximize its benefits and minimize its risks. As research continues, new insights into its mechanisms and applications will further refine its role in clinical practice.
Cortisol succinate Mechanism of Action
The mechanism of action of cortisol succinate involves its role as a synthetic analog of cortisol, a hormone produced by the adrenal cortex. Cortisol plays a vital role in various physiological processes, including the regulation of metabolism, immune response, and stress responses. When administered, cortisol succinate binds to glucocorticoid receptors in the cytoplasm of target cells. This binding initiates a cascade of events that lead to the modulation of gene expression. Specifically, cortisol succinate influences the transcription of anti-inflammatory proteins and the repression of pro-inflammatory genes. This dual action contributes to its potent anti-inflammatory and immunosuppressive properties. Additionally, cortisol succinate stabilizes cell membranes and lysosomal membranes, reducing the release of inflammatory mediators. It also promotes gluconeogenesis, enhances the breakdown of lipids, and influences the distribution of white blood cells, which collectively contribute to its broad-spectrum therapeutic effects.
How to Use Cortisol succinate
Cortisol succinate can be administered through various routes depending on the clinical scenario. The most common methods include intravenous (IV) and intramuscular (IM) injections. The choice of administration depends on the urgency and severity of the condition being treated. Intravenous administration is generally preferred in emergency situations, such as severe asthma attacks or adrenal crisis, due to its rapid onset of action, typically within minutes. Intramuscular injections, on the other hand, provide a more sustained release of the drug and are useful in situations where immediate onset is not as critical.
The dosage of cortisol succinate varies widely based on the condition being treated, the patient's age, and their overall health status. For instance, in the management of acute asthma exacerbations, adult dosages may range from 100 mg to 500 mg administered intravenously every 2 to 6 hours, whereas for adrenal insufficiency, a typical regimen might involve lower dosages given at regular intervals. It is crucial for healthcare providers to individualize the dosing and administration schedule to optimize therapeutic outcomes while minimizing potential side effects.
Patients receiving cortisol succinate should be monitored closely for their response to therapy, and adjustments may be necessary based on clinical feedback. Tapering the dose gradually is often recommended when discontinuing the drug to avoid adrenal insufficiency resulting from sudden withdrawal.
What is Cortisol succinate Side Effects
While cortisol succinate is highly effective in managing a range of inflammatory and autoimmune conditions, its use is not without potential side effects. The side effects can be categorized into short-term and long-term effects.
Short-term side effects may include elevated blood sugar levels, fluid retention, high blood pressure, and mood changes such as irritability or euphoria. Gastrointestinal disturbances, such as nausea and vomiting, may also occur. In some cases, patients may experience a condition known as "steroid-induced psychosis," characterized by changes in mental status, including confusion, hallucinations, and severe mood swings.
Long-term use of cortisol succinate carries a risk of more serious side effects. These include osteoporosis, muscle wasting, and increased susceptibility to infections due to immunosuppression. Prolonged treatment can also lead to the development of Cushing's syndrome, characterized by a round face, central obesity, and skin changes such as striae and bruising. Additionally, chronic use can result in adrenal suppression, where the body's natural cortisol production is inhibited, making it challenging to respond to stress.
Contraindications for the use of cortisol succinate include systemic fungal infections and known hypersensitivity to the drug. Caution is advised in patients with conditions such as diabetes, hypertension, peptic ulcer disease, and psychiatric disorders, as cortisol succinate can exacerbate these conditions. Pregnant and breastfeeding women should use the drug only when clearly needed, as it can cross the placenta and be excreted in breast milk.
What Other Drugs Will Affect Cortisol succinate
The efficacy and safety of cortisol succinate can be influenced by concomitant use of other drugs. Drug interactions can either potentiate its effects, increasing the risk of side effects, or diminish its therapeutic efficacy.
Drugs that induce hepatic enzymes, such as phenytoin, phenobarbital, and rifampin, can increase the metabolism of cortisol succinate, potentially reducing its effectiveness. On the other hand, drugs that inhibit hepatic enzymes, such as ketoconazole and certain antibiotics like erythromycin, can decrease the metabolism of cortisol succinate, increasing the risk of toxicity.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, when used concurrently with cortisol succinate, can increase the risk of gastrointestinal bleeding and ulceration. This combination should be used with caution, and protective measures such as the use of proton pump inhibitors may be considered.
Additionally, diuretics, particularly thiazides and loop diuretics, can exacerbate the hypokalemic effects of cortisol succinate, leading to significant potassium depletion. Patients on such regimens should have their electrolyte levels monitored closely.
Vaccines may also interact with cortisol succinate. Live vaccines, in particular, should be avoided in patients receiving immunosuppressive doses of the drug, as their immune response may be inadequate, and there is a risk of disseminated infection.
In summary, while cortisol succinate is a powerful and versatile drug in the management of various inflammatory and autoimmune conditions, its use requires careful consideration of potential side effects and drug interactions. Close monitoring and individualized dosing are essential to maximize its benefits and minimize its risks. As research continues, new insights into its mechanisms and applications will further refine its role in clinical practice.
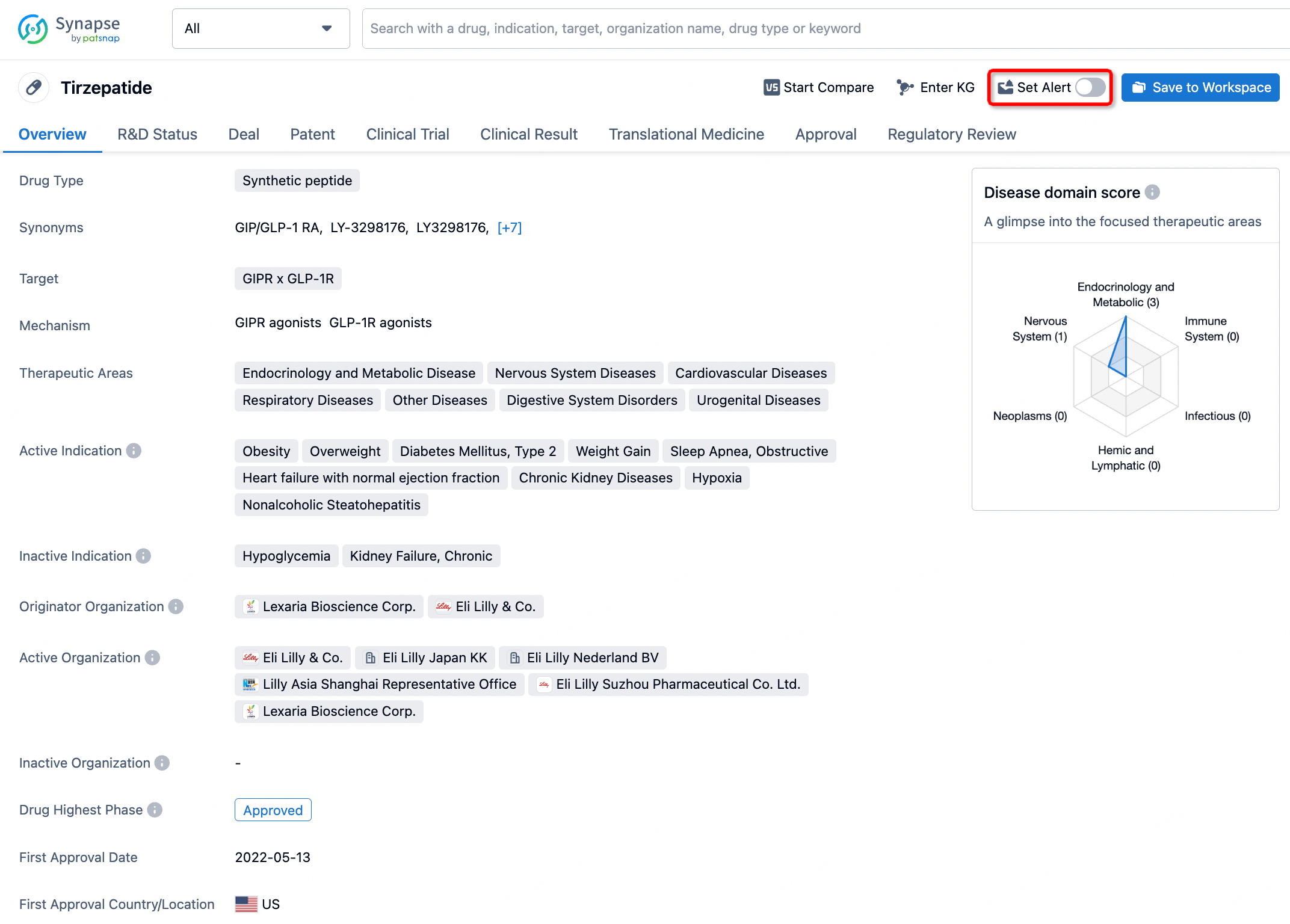
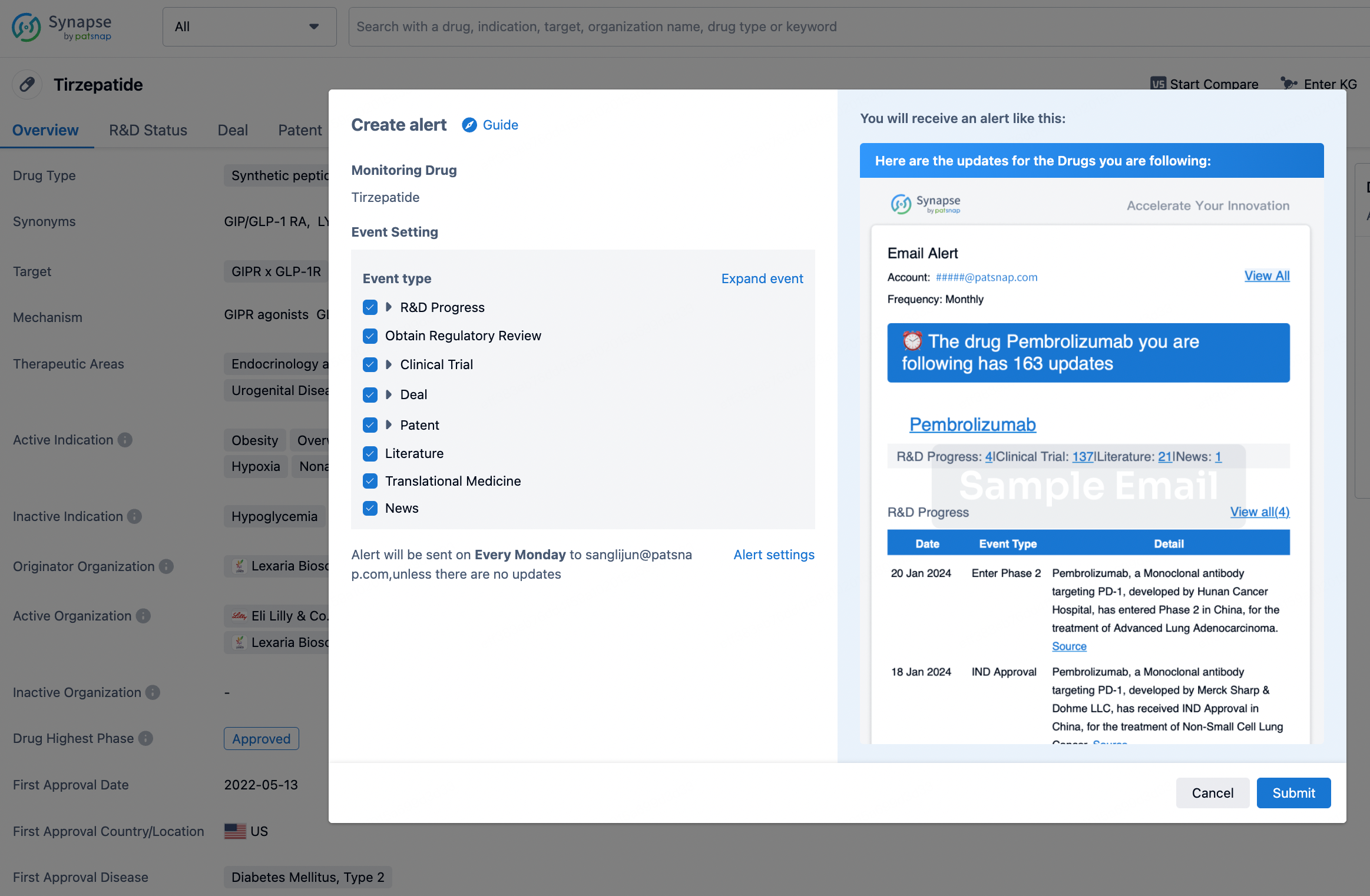
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.