Request Demo
What is Flurithromycin used for?
14 June 2024
Flurithromycin is a relatively new player in the world of antibiotics, but it has already shown significant promise in combating bacterial infections. This macrolide antibiotic functions similarly to other drugs in its class, such as erythromycin and azithromycin, but it has distinct advantages that make it especially compelling. Developed through the collaborative efforts of several research institutions, flurithromycin has undergone rigorous testing and research to ensure its efficacy and safety. Trade names for flurithromycin are still under consideration as it is in the advanced stages of clinical trials, but it has already garnered attention for its potential applications. The drug primarily targets bacterial ribosomes, inhibiting protein synthesis and thereby stymying bacterial growth. Indications for flurithromycin include respiratory tract infections, skin infections, and other bacterial infections. Research progress has been promising, with numerous studies indicating its effectiveness and fewer side effects compared to older antibiotics in the macrolide family.
Flurithromycin Mechanism of Action
Understanding how flurithromycin works requires a fundamental grasp of bacterial biology and antibiotic mechanisms. Like other macrolides, flurithromycin targets the bacterial ribosome, a crucial component of the protein synthesis machinery. Specifically, it binds to the 50S subunit of the ribosome, leading to a blockade in the translocation step of protein synthesis. This interruption prevents the bacteria from producing essential proteins needed for their growth and replication.
Flurithromycin's unique structure provides it with enhanced binding affinity to the ribosome, which translates to increased potency against a broad spectrum of bacteria. This enhanced binding is partly due to the fluorine atom incorporated into its molecular structure, which sets it apart from older macrolides. The addition of the fluorine atom improves the drug's stability and tissue penetration, allowing it to effectively reach and maintain therapeutic levels at the site of infection.
Furthermore, flurithromycin exhibits an extended half-life, which means it can maintain effective concentrations in the body for a longer duration. This property not only improves patient compliance by reducing the frequency of doses but also ensures a more consistent eradication of the bacterial pathogens.
How to Use Flurithromycin
Flurithromycin is typically administered orally in the form of tablets or capsules, and it is also available as an intravenous solution for severe infections requiring hospital treatment. The oral formulation is generally the preferred method for mild to moderate infections due to its convenience and efficacy. The drug is well absorbed through the gastrointestinal tract, achieving peak plasma concentrations within 1 to 2 hours after administration.
The onset of action for flurithromycin is relatively rapid, with patients often experiencing symptom relief within 24 to 48 hours of starting the medication. For most bacterial infections, the standard dosage regimen involves taking the medication once daily, usually for a duration of 5 to 10 days, depending on the severity and type of infection.
It is crucial to complete the entire prescribed course of flurithromycin, even if symptoms improve before the medication is finished. Premature discontinuation can lead to incomplete eradication of the bacteria and may contribute to the development of antibiotic resistance.
Patients are advised to take flurithromycin with or without food, although taking it with food may help to minimize gastrointestinal discomfort. It is essential to follow the healthcare provider's instructions regarding the dosage and duration of treatment to ensure optimal outcomes.
What are Flurithromycin Side Effects
As with any medication, flurithromycin can cause side effects, although not everyone will experience them. The most common side effects include gastrointestinal disturbances such as nausea, vomiting, diarrhea, and abdominal pain. These symptoms are typically mild and transient, resolving on their own without the need for medical intervention.
Some patients may experience more severe side effects, such as allergic reactions manifesting as rash, itching, or difficulty breathing. In such cases, it is imperative to seek immediate medical attention. Additionally, flurithromycin can cause alterations in liver enzyme levels, so it is essential to monitor liver function in patients with pre-existing liver conditions or those taking other hepatotoxic medications.
One of the notable advantages of flurithromycin is its lower incidence of cardiac side effects compared to other macrolides. While drugs like erythromycin and azithromycin are associated with an increased risk of QT prolongation and arrhythmias, flurithromycin has shown a more favorable cardiac safety profile in clinical studies.
Contraindications for flurithromycin include known hypersensitivity to macrolide antibiotics and severe hepatic impairment. Patients with a history of antibiotic-associated colitis should use flurithromycin with caution, as it may exacerbate the condition.
What Other Drugs Will Affect Flurithromycin
Flurithromycin, like many other antibiotics, can interact with a variety of medications, potentially altering their effects or increasing the risk of adverse reactions. One of the primary concerns with macrolide antibiotics is their potential to inhibit the cytochrome P450 enzyme system, particularly CYP3A4. This enzyme is responsible for the metabolism of many drugs, and inhibition by flurithromycin can lead to increased levels of co-administered medications.
Drugs that may be affected by this interaction include statins, which are used to lower cholesterol levels. Concurrent use of flurithromycin with statins, particularly those metabolized by CYP3A4 (such as simvastatin and atorvastatin), can increase the risk of statin-related side effects, including myopathy and rhabdomyolysis. Patients taking these medications should be closely monitored, and dose adjustments may be necessary.
Another group of drugs that can interact with flurithromycin includes oral anticoagulants like warfarin. Flurithromycin can enhance the anticoagulant effect of warfarin, leading to an increased risk of bleeding. Regular monitoring of INR (International Normalized Ratio) is essential in patients taking both medications, and dose adjustments of warfarin may be required.
Additionally, flurithromycin may interact with other antibiotics and antifungal agents, such as rifampin and ketoconazole, which can either increase or decrease its efficacy. Close monitoring and potential dose adjustments are necessary when these drugs are used concomitantly.
In conclusion, flurithromycin represents a promising advancement in the field of antibiotics, offering potent antibacterial activity with a favorable safety profile. Its unique mechanism of action, combined with its convenient dosing regimen and rapid onset of action, makes it a valuable option for treating various bacterial infections. However, as with any medication, it is essential to be aware of potential side effects, contraindications, and drug interactions to ensure safe and effective use. As research continues and clinical experience with flurithromycin expands, it is likely to become an increasingly important tool in our arsenal against bacterial infections.
Flurithromycin Mechanism of Action
Understanding how flurithromycin works requires a fundamental grasp of bacterial biology and antibiotic mechanisms. Like other macrolides, flurithromycin targets the bacterial ribosome, a crucial component of the protein synthesis machinery. Specifically, it binds to the 50S subunit of the ribosome, leading to a blockade in the translocation step of protein synthesis. This interruption prevents the bacteria from producing essential proteins needed for their growth and replication.
Flurithromycin's unique structure provides it with enhanced binding affinity to the ribosome, which translates to increased potency against a broad spectrum of bacteria. This enhanced binding is partly due to the fluorine atom incorporated into its molecular structure, which sets it apart from older macrolides. The addition of the fluorine atom improves the drug's stability and tissue penetration, allowing it to effectively reach and maintain therapeutic levels at the site of infection.
Furthermore, flurithromycin exhibits an extended half-life, which means it can maintain effective concentrations in the body for a longer duration. This property not only improves patient compliance by reducing the frequency of doses but also ensures a more consistent eradication of the bacterial pathogens.
How to Use Flurithromycin
Flurithromycin is typically administered orally in the form of tablets or capsules, and it is also available as an intravenous solution for severe infections requiring hospital treatment. The oral formulation is generally the preferred method for mild to moderate infections due to its convenience and efficacy. The drug is well absorbed through the gastrointestinal tract, achieving peak plasma concentrations within 1 to 2 hours after administration.
The onset of action for flurithromycin is relatively rapid, with patients often experiencing symptom relief within 24 to 48 hours of starting the medication. For most bacterial infections, the standard dosage regimen involves taking the medication once daily, usually for a duration of 5 to 10 days, depending on the severity and type of infection.
It is crucial to complete the entire prescribed course of flurithromycin, even if symptoms improve before the medication is finished. Premature discontinuation can lead to incomplete eradication of the bacteria and may contribute to the development of antibiotic resistance.
Patients are advised to take flurithromycin with or without food, although taking it with food may help to minimize gastrointestinal discomfort. It is essential to follow the healthcare provider's instructions regarding the dosage and duration of treatment to ensure optimal outcomes.
What are Flurithromycin Side Effects
As with any medication, flurithromycin can cause side effects, although not everyone will experience them. The most common side effects include gastrointestinal disturbances such as nausea, vomiting, diarrhea, and abdominal pain. These symptoms are typically mild and transient, resolving on their own without the need for medical intervention.
Some patients may experience more severe side effects, such as allergic reactions manifesting as rash, itching, or difficulty breathing. In such cases, it is imperative to seek immediate medical attention. Additionally, flurithromycin can cause alterations in liver enzyme levels, so it is essential to monitor liver function in patients with pre-existing liver conditions or those taking other hepatotoxic medications.
One of the notable advantages of flurithromycin is its lower incidence of cardiac side effects compared to other macrolides. While drugs like erythromycin and azithromycin are associated with an increased risk of QT prolongation and arrhythmias, flurithromycin has shown a more favorable cardiac safety profile in clinical studies.
Contraindications for flurithromycin include known hypersensitivity to macrolide antibiotics and severe hepatic impairment. Patients with a history of antibiotic-associated colitis should use flurithromycin with caution, as it may exacerbate the condition.
What Other Drugs Will Affect Flurithromycin
Flurithromycin, like many other antibiotics, can interact with a variety of medications, potentially altering their effects or increasing the risk of adverse reactions. One of the primary concerns with macrolide antibiotics is their potential to inhibit the cytochrome P450 enzyme system, particularly CYP3A4. This enzyme is responsible for the metabolism of many drugs, and inhibition by flurithromycin can lead to increased levels of co-administered medications.
Drugs that may be affected by this interaction include statins, which are used to lower cholesterol levels. Concurrent use of flurithromycin with statins, particularly those metabolized by CYP3A4 (such as simvastatin and atorvastatin), can increase the risk of statin-related side effects, including myopathy and rhabdomyolysis. Patients taking these medications should be closely monitored, and dose adjustments may be necessary.
Another group of drugs that can interact with flurithromycin includes oral anticoagulants like warfarin. Flurithromycin can enhance the anticoagulant effect of warfarin, leading to an increased risk of bleeding. Regular monitoring of INR (International Normalized Ratio) is essential in patients taking both medications, and dose adjustments of warfarin may be required.
Additionally, flurithromycin may interact with other antibiotics and antifungal agents, such as rifampin and ketoconazole, which can either increase or decrease its efficacy. Close monitoring and potential dose adjustments are necessary when these drugs are used concomitantly.
In conclusion, flurithromycin represents a promising advancement in the field of antibiotics, offering potent antibacterial activity with a favorable safety profile. Its unique mechanism of action, combined with its convenient dosing regimen and rapid onset of action, makes it a valuable option for treating various bacterial infections. However, as with any medication, it is essential to be aware of potential side effects, contraindications, and drug interactions to ensure safe and effective use. As research continues and clinical experience with flurithromycin expands, it is likely to become an increasingly important tool in our arsenal against bacterial infections.
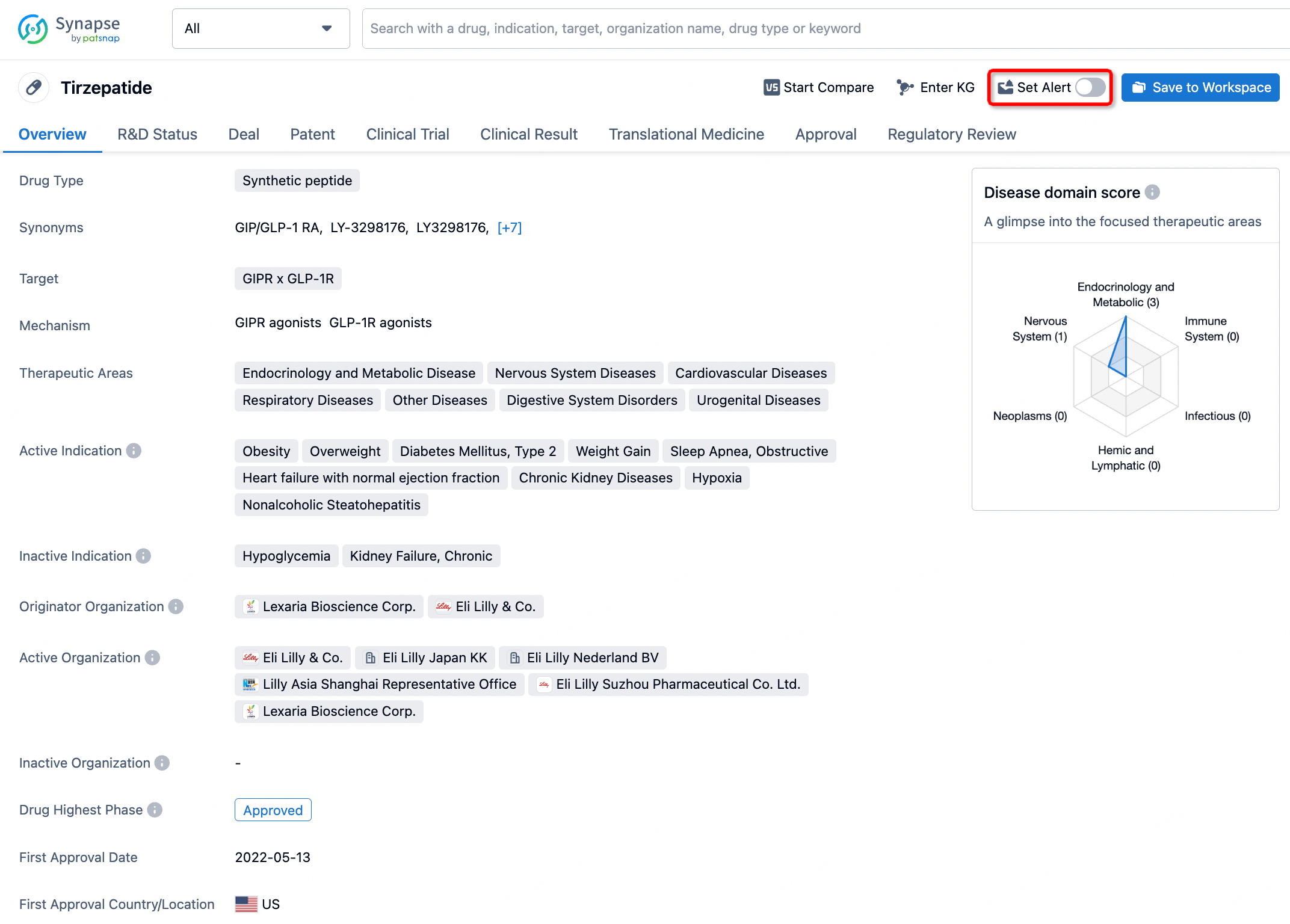
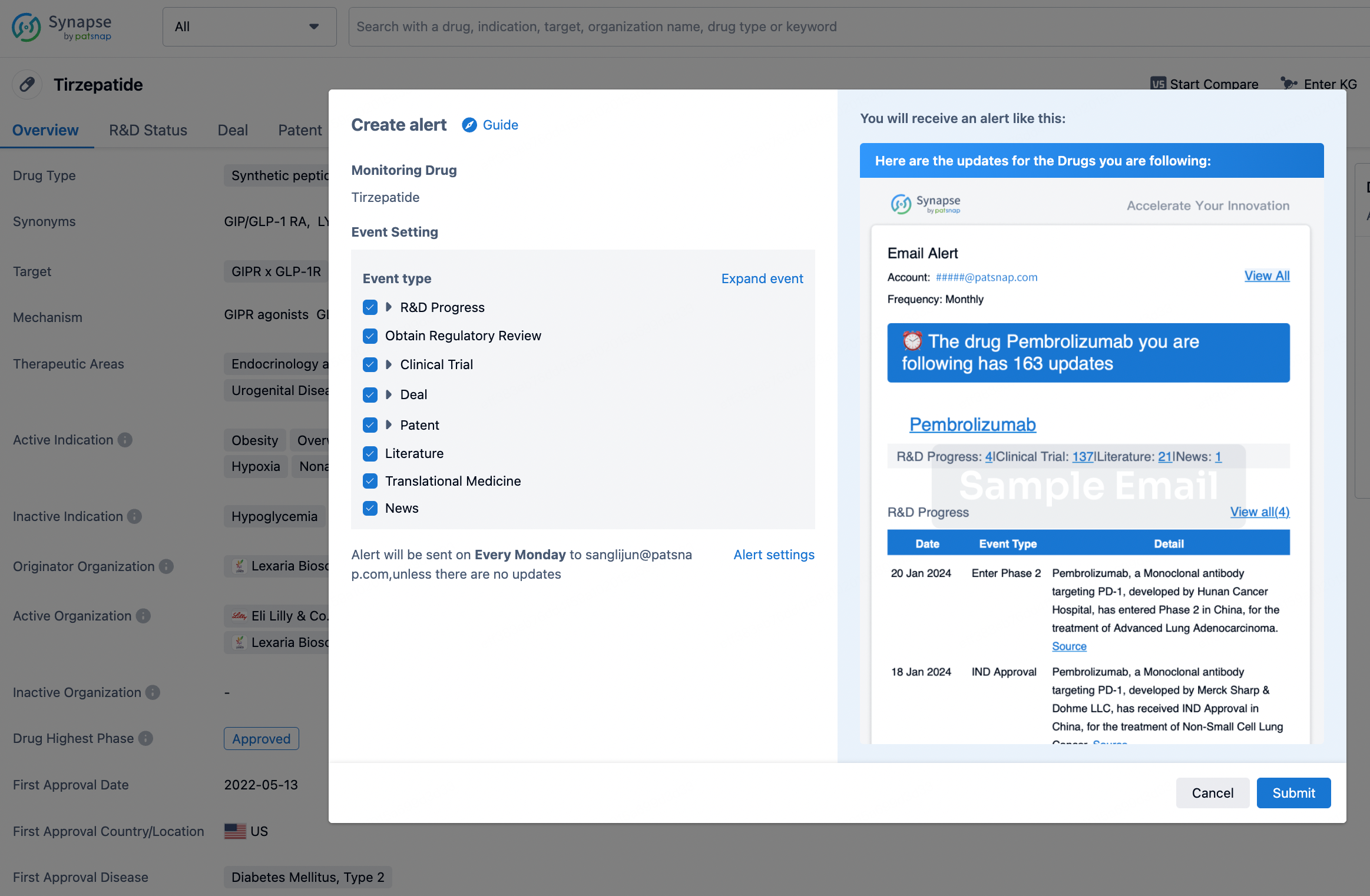
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.