Request Demo
What are PBPs inhibitors and how do they work?
21 June 2024
Penicillin-binding proteins (PBPs) inhibitors are a crucial class of antibiotics that have revolutionized the treatment of bacterial infections. These drugs specifically target PBPs, which are essential enzymes involved in the synthesis of bacterial cell walls. Understanding the mechanism of action, applications, and significance of PBP inhibitors can provide insight into their vital role in modern medicine.
PBPs are a group of enzymes found in bacteria that are essential for the synthesis and maintenance of the bacterial cell wall. The cell wall is a critical structure that provides shape and rigidity to the bacteria, protecting them from external pressures and preventing lysis. PBPs catalyze the final stages of peptidoglycan synthesis, a key component of the bacterial cell wall. They are named for their ability to bind to penicillin and related antibiotics. When PBPs are inhibited, the integrity of the bacterial cell wall is compromised, leading to cell death. This makes PBPs a valuable target for antibiotic therapy.
PBPs inhibitors work by binding to the active site of PBPs, thereby preventing them from performing their normal enzymatic function. The most well-known PBPs inhibitors are the β-lactam antibiotics, which include penicillins, cephalosporins, carbapenems, and monobactams. These antibiotics share a common β-lactam ring structure, which is essential for their binding to PBPs.
When a β-lactam antibiotic binds to a PBP, it forms a stable, covalent complex that inhibits the enzyme's activity. This inhibition prevents the cross-linking of peptidoglycan chains, leading to the accumulation of unlinked peptidoglycan precursors. As a result, the cell wall becomes weakened and unable to withstand osmotic pressure, causing the bacterial cell to lyse and die. This bactericidal effect is particularly effective against actively dividing bacteria, which rely heavily on PBPs for cell wall synthesis and remodeling.
Other classes of PBPs inhibitors include non-β-lactam drugs such as glycopeptides (e.g., vancomycin) and lipopeptides (e.g., daptomycin), which also disrupt cell wall synthesis but through different mechanisms. These drugs are often used as alternatives to β-lactams, especially in cases of resistance or allergy.
PBPs inhibitors are used to treat a wide range of bacterial infections. Their broad-spectrum activity makes them effective against many Gram-positive and Gram-negative bacteria. Some of the common clinical applications of PBPs inhibitors include:
1. **Respiratory Tract Infections**: PBPs inhibitors are frequently used to treat bacterial pneumonia, bronchitis, and sinusitis. For example, penicillin and amoxicillin are commonly prescribed for Streptococcus pneumoniae and Haemophilus influenzae infections.
2. **Skin and Soft Tissue Infections**: Cephalosporins and other PBPs inhibitors are effective against skin infections such as cellulitis, impetigo, and abscesses caused by Staphylococcus aureus and Streptococcus pyogenes.
3. **Urinary Tract Infections (UTIs)**: PBPs inhibitors like amoxicillin-clavulanate and cephalexin are commonly used to treat UTIs caused by Escherichia coli and other susceptible bacteria.
4. **Meningitis**: Certain PBPs inhibitors, such as third-generation cephalosporins (e.g., ceftriaxone, cefotaxime), are used to treat bacterial meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae.
5. **Gonorrhea**: The carbapenem antibiotic ertapenem is used to treat multidrug-resistant Neisseria gonorrhoeae infections.
6. **Sepsis and Endocarditis**: PBPs inhibitors are crucial in the management of severe infections like sepsis and bacterial endocarditis, often caused by Staphylococcus aureus and Enterococcus species.
7. **Surgical Prophylaxis**: To prevent postoperative infections, PBPs inhibitors like cefazolin are administered prophylactically before certain surgical procedures.
In conclusion, PBPs inhibitors have transformed the landscape of bacterial infection treatment. By targeting the essential bacterial cell wall synthesis machinery, these drugs are able to effectively eradicate a wide variety of pathogenic bacteria. Their broad-spectrum efficacy and versatility make them indispensable in clinical settings. However, the rise of antibiotic resistance underscores the need for continued research and development of new PBPs inhibitors and alternative therapies. Through ongoing innovation and vigilance, the medical community can continue to harness the power of PBP inhibitors to combat bacterial infections and improve public health outcomes.
PBPs are a group of enzymes found in bacteria that are essential for the synthesis and maintenance of the bacterial cell wall. The cell wall is a critical structure that provides shape and rigidity to the bacteria, protecting them from external pressures and preventing lysis. PBPs catalyze the final stages of peptidoglycan synthesis, a key component of the bacterial cell wall. They are named for their ability to bind to penicillin and related antibiotics. When PBPs are inhibited, the integrity of the bacterial cell wall is compromised, leading to cell death. This makes PBPs a valuable target for antibiotic therapy.
PBPs inhibitors work by binding to the active site of PBPs, thereby preventing them from performing their normal enzymatic function. The most well-known PBPs inhibitors are the β-lactam antibiotics, which include penicillins, cephalosporins, carbapenems, and monobactams. These antibiotics share a common β-lactam ring structure, which is essential for their binding to PBPs.
When a β-lactam antibiotic binds to a PBP, it forms a stable, covalent complex that inhibits the enzyme's activity. This inhibition prevents the cross-linking of peptidoglycan chains, leading to the accumulation of unlinked peptidoglycan precursors. As a result, the cell wall becomes weakened and unable to withstand osmotic pressure, causing the bacterial cell to lyse and die. This bactericidal effect is particularly effective against actively dividing bacteria, which rely heavily on PBPs for cell wall synthesis and remodeling.
Other classes of PBPs inhibitors include non-β-lactam drugs such as glycopeptides (e.g., vancomycin) and lipopeptides (e.g., daptomycin), which also disrupt cell wall synthesis but through different mechanisms. These drugs are often used as alternatives to β-lactams, especially in cases of resistance or allergy.
PBPs inhibitors are used to treat a wide range of bacterial infections. Their broad-spectrum activity makes them effective against many Gram-positive and Gram-negative bacteria. Some of the common clinical applications of PBPs inhibitors include:
1. **Respiratory Tract Infections**: PBPs inhibitors are frequently used to treat bacterial pneumonia, bronchitis, and sinusitis. For example, penicillin and amoxicillin are commonly prescribed for Streptococcus pneumoniae and Haemophilus influenzae infections.
2. **Skin and Soft Tissue Infections**: Cephalosporins and other PBPs inhibitors are effective against skin infections such as cellulitis, impetigo, and abscesses caused by Staphylococcus aureus and Streptococcus pyogenes.
3. **Urinary Tract Infections (UTIs)**: PBPs inhibitors like amoxicillin-clavulanate and cephalexin are commonly used to treat UTIs caused by Escherichia coli and other susceptible bacteria.
4. **Meningitis**: Certain PBPs inhibitors, such as third-generation cephalosporins (e.g., ceftriaxone, cefotaxime), are used to treat bacterial meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae.
5. **Gonorrhea**: The carbapenem antibiotic ertapenem is used to treat multidrug-resistant Neisseria gonorrhoeae infections.
6. **Sepsis and Endocarditis**: PBPs inhibitors are crucial in the management of severe infections like sepsis and bacterial endocarditis, often caused by Staphylococcus aureus and Enterococcus species.
7. **Surgical Prophylaxis**: To prevent postoperative infections, PBPs inhibitors like cefazolin are administered prophylactically before certain surgical procedures.
In conclusion, PBPs inhibitors have transformed the landscape of bacterial infection treatment. By targeting the essential bacterial cell wall synthesis machinery, these drugs are able to effectively eradicate a wide variety of pathogenic bacteria. Their broad-spectrum efficacy and versatility make them indispensable in clinical settings. However, the rise of antibiotic resistance underscores the need for continued research and development of new PBPs inhibitors and alternative therapies. Through ongoing innovation and vigilance, the medical community can continue to harness the power of PBP inhibitors to combat bacterial infections and improve public health outcomes.
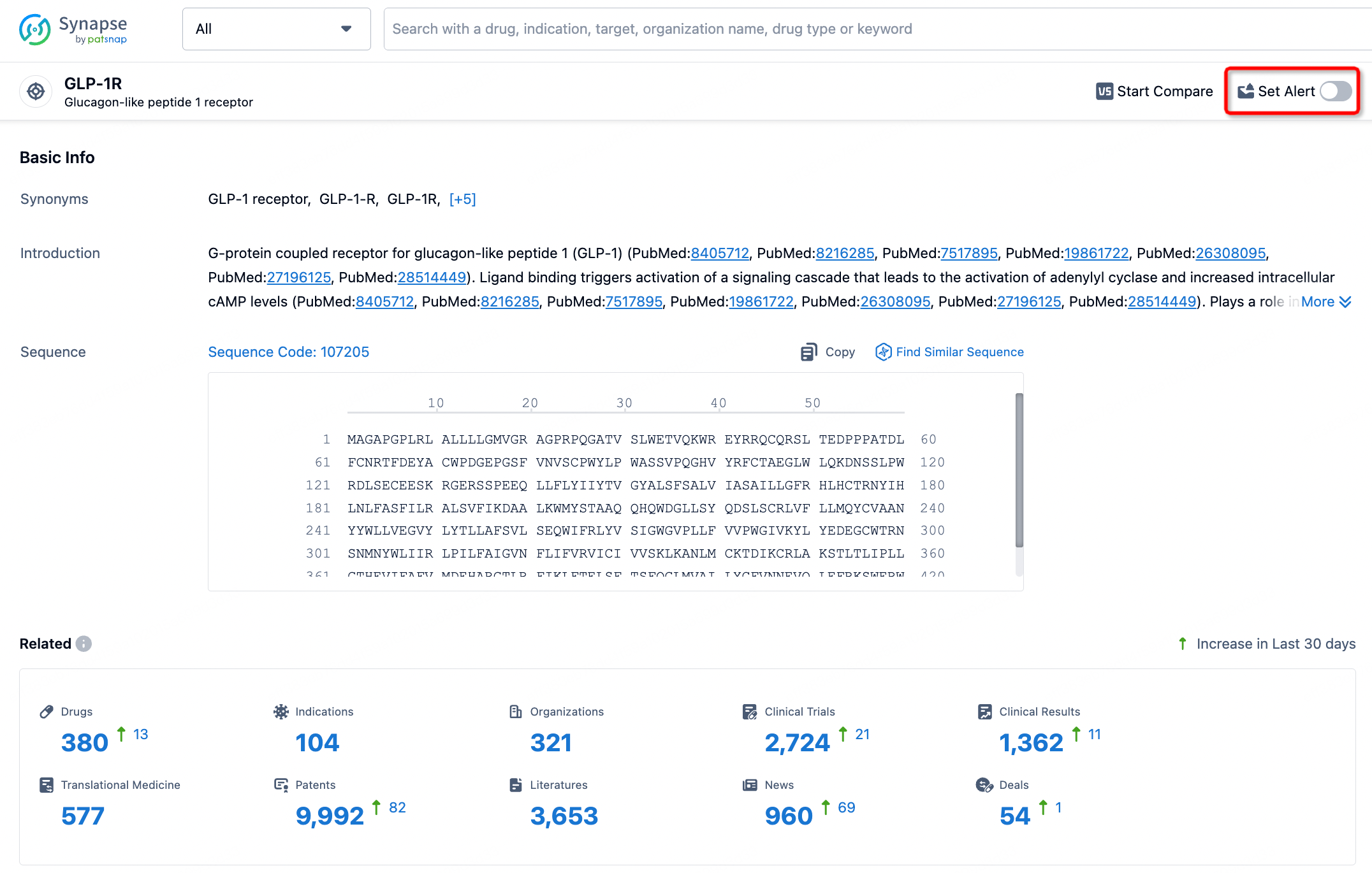
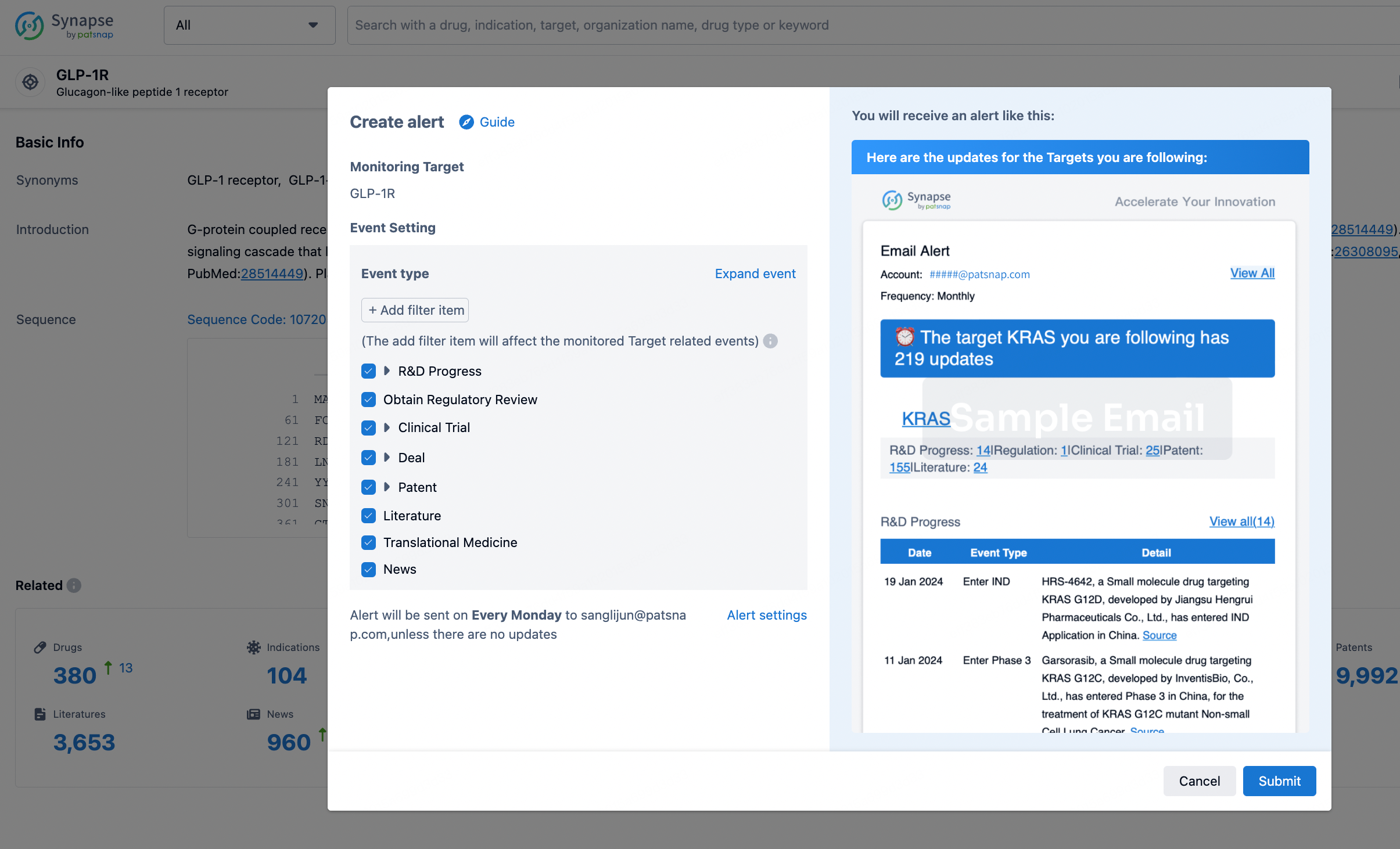
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.