Request Demo
What is Phenytoin used for?
15 June 2024
Phenytoin: An Overview
Phenytoin, commonly known by its trade names such as Dilantin and Phenytek, is a widely recognized anticonvulsant drug primarily used to manage and prevent seizures. It has been a cornerstone in the treatment of epilepsy for decades. Developed in the early 20th century, Phenytoin has since been extensively studied and is one of the most well-understood antiepileptic drugs on the market. Phenytoin is utilized in various clinical settings, primarily for its effectiveness in controlling generalized tonic-clonic (grand mal) and complex partial seizures.
Beyond epilepsy, Phenytoin has also found applications in treating certain types of arrhythmias and trigeminal neuralgia, though these uses are less common. The drug functions by stabilizing neuronal membranes and reducing repetitive neuronal firing. The extensive research conducted by numerous institutions worldwide has solidified Phenytoin's place in modern medicine, despite the emergence of newer antiepileptic drugs. The continued research into its efficacy and safety profile ensures that Phenytoin remains a relevant and essential medication in treating neurological disorders.
Phenytoin Mechanism of Action
The mechanism of action of Phenytoin is well-studied and understood. Phenytoin primarily works by blocking voltage-gated sodium channels in the brain and spinal cord. By doing so, it stabilizes the neuronal membrane and prevents the repetitive firing of action potentials. This reduction in excitatory activity is crucial in preventing the abnormal electrical discharges that characterize seizures.
Phenytoin achieves this by selectively binding to the inactive form of the sodium channel, prolonging its inactivated state and thus reducing neuronal excitability. This action makes Phenytoin particularly effective in managing generalized tonic-clonic seizures and complex partial seizures. Moreover, Phenytoin has a lesser but notable effect on calcium channels and the release of neurotransmitters such as glutamate, further contributing to its anticonvulsant properties.
Overall, the ability of Phenytoin to modulate neuronal activity and prevent excessive firing makes it a potent and reliable option for seizure control.
How to Use Phenytoin
Phenytoin is available in various forms, including oral tablets, extended-release capsules, chewable tablets, and injectable solutions, providing flexibility in administration to suit different patient needs. The method of drug administration depends on the clinical scenario and patient-specific factors.
For oral administration, Phenytoin is typically taken once or twice daily, depending on the formulation. Extended-release capsules are usually preferred for their convenience and consistent drug levels. The onset of action for oral Phenytoin is relatively slow, with peak plasma levels reached within 4 to 12 hours after ingestion. This slow onset is advantageous for maintaining stable drug levels and minimizing side effects.
Injectable Phenytoin is used in acute settings, such as during a status epilepticus episode, where rapid control of seizures is required. When administered intravenously, the drug takes effect within 30 minutes. However, IV administration must be done carefully due to the risk of hypotension and arrhythmias if infused too quickly.
Dosage adjustments are often necessary based on therapeutic drug monitoring, as Phenytoin has a narrow therapeutic index. Monitoring plasma levels helps ensure efficacy while minimizing the risk of toxicity. The recommended therapeutic range for Phenytoin is typically between 10-20 µg/mL.
Adherence to prescribed dosing schedules is critical for optimal seizure control, and sudden discontinuation of Phenytoin should be avoided to prevent withdrawal seizures.
Phenytoin Side Effects
While Phenytoin is effective in managing seizures, it is not without potential side effects. Common side effects include dizziness, drowsiness, nausea, vomiting, constipation, and gingival hyperplasia (overgrowth of gum tissue). These side effects are generally dose-dependent and may be minimized by proper dose adjustment and adherence to the prescribed regimen.
More severe side effects can occur, particularly with long-term use. These include osteomalacia (softening of the bones), folate deficiency leading to megaloblastic anemia, and peripheral neuropathy. Chronic use of Phenytoin can also lead to cosmetic issues such as hirsutism (excessive hair growth) and acne.
Phenytoin has several contraindications. It should not be used in individuals with a known hypersensitivity to the drug or its components. Patients with a history of hepatotoxicity related to Phenytoin, or those with specific cardiac conditions like bradycardia or heart block, should avoid its use unless absolutely necessary and under close supervision.
One of the more serious risks associated with Phenytoin is the potential for Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), rare but life-threatening skin reactions. These risks are higher in individuals with certain genetic profiles, particularly those of Asian descent carrying the HLA-B*1502 allele. Genetic screening can help mitigate this risk.
Another important consideration is the drug’s potential impact on mental health, as it can cause mood changes, agitation, and, in rare cases, suicidal ideation.
What Other Drugs Will Affect Phenytoin
Phenytoin is known for its potential to interact with numerous other medications, which can either increase its toxicity or reduce its efficacy. It is metabolized by the cytochrome P450 enzyme system, specifically CYP2C9 and CYP2C19, making it susceptible to interactions with drugs that induce or inhibit these enzymes.
Enzyme inducers such as carbamazepine, phenobarbital, and rifampin can decrease Phenytoin levels, potentially leading to subtherapeutic effects and increased seizure risk. Conversely, enzyme inhibitors like valproic acid, cimetidine, and fluoxetine can increase Phenytoin levels, raising the risk of toxicity.
Other anticonvulsants can also interact with Phenytoin. For instance, valproic acid not only inhibits Phenytoin metabolism but also displaces it from plasma proteins, further increasing free Phenytoin levels.
Warfarin, a commonly used anticoagulant, is another drug that heavily interacts with Phenytoin. Both drugs can affect each other's metabolism, leading to either increased bleeding risk or reduced anticoagulant effect, necessitating close monitoring of coagulation parameters.
Oral contraceptives can be less effective when taken with Phenytoin due to its enzyme-inducing properties, which can increase the metabolism of estrogen and progesterone. This interaction necessitates the use of alternative or additional contraceptive methods.
Alcohol consumption can also influence Phenytoin levels. Acute alcohol intake can inhibit its metabolism, while chronic alcohol use can induce enzyme activity, leading to variable effects.
Patients should always inform their healthcare providers about all medications they are taking, including over-the-counter drugs and supplements, to carefully manage and adjust doses and avoid potential interactions.
In summary, while Phenytoin remains a vital tool in the management of epilepsy and other neurological conditions, its use requires careful monitoring and consideration of potential side effects and drug interactions. Proper patient education and regular follow-ups are essential to optimize therapeutic outcomes and minimize risks.
Phenytoin, commonly known by its trade names such as Dilantin and Phenytek, is a widely recognized anticonvulsant drug primarily used to manage and prevent seizures. It has been a cornerstone in the treatment of epilepsy for decades. Developed in the early 20th century, Phenytoin has since been extensively studied and is one of the most well-understood antiepileptic drugs on the market. Phenytoin is utilized in various clinical settings, primarily for its effectiveness in controlling generalized tonic-clonic (grand mal) and complex partial seizures.
Beyond epilepsy, Phenytoin has also found applications in treating certain types of arrhythmias and trigeminal neuralgia, though these uses are less common. The drug functions by stabilizing neuronal membranes and reducing repetitive neuronal firing. The extensive research conducted by numerous institutions worldwide has solidified Phenytoin's place in modern medicine, despite the emergence of newer antiepileptic drugs. The continued research into its efficacy and safety profile ensures that Phenytoin remains a relevant and essential medication in treating neurological disorders.
Phenytoin Mechanism of Action
The mechanism of action of Phenytoin is well-studied and understood. Phenytoin primarily works by blocking voltage-gated sodium channels in the brain and spinal cord. By doing so, it stabilizes the neuronal membrane and prevents the repetitive firing of action potentials. This reduction in excitatory activity is crucial in preventing the abnormal electrical discharges that characterize seizures.
Phenytoin achieves this by selectively binding to the inactive form of the sodium channel, prolonging its inactivated state and thus reducing neuronal excitability. This action makes Phenytoin particularly effective in managing generalized tonic-clonic seizures and complex partial seizures. Moreover, Phenytoin has a lesser but notable effect on calcium channels and the release of neurotransmitters such as glutamate, further contributing to its anticonvulsant properties.
Overall, the ability of Phenytoin to modulate neuronal activity and prevent excessive firing makes it a potent and reliable option for seizure control.
How to Use Phenytoin
Phenytoin is available in various forms, including oral tablets, extended-release capsules, chewable tablets, and injectable solutions, providing flexibility in administration to suit different patient needs. The method of drug administration depends on the clinical scenario and patient-specific factors.
For oral administration, Phenytoin is typically taken once or twice daily, depending on the formulation. Extended-release capsules are usually preferred for their convenience and consistent drug levels. The onset of action for oral Phenytoin is relatively slow, with peak plasma levels reached within 4 to 12 hours after ingestion. This slow onset is advantageous for maintaining stable drug levels and minimizing side effects.
Injectable Phenytoin is used in acute settings, such as during a status epilepticus episode, where rapid control of seizures is required. When administered intravenously, the drug takes effect within 30 minutes. However, IV administration must be done carefully due to the risk of hypotension and arrhythmias if infused too quickly.
Dosage adjustments are often necessary based on therapeutic drug monitoring, as Phenytoin has a narrow therapeutic index. Monitoring plasma levels helps ensure efficacy while minimizing the risk of toxicity. The recommended therapeutic range for Phenytoin is typically between 10-20 µg/mL.
Adherence to prescribed dosing schedules is critical for optimal seizure control, and sudden discontinuation of Phenytoin should be avoided to prevent withdrawal seizures.
Phenytoin Side Effects
While Phenytoin is effective in managing seizures, it is not without potential side effects. Common side effects include dizziness, drowsiness, nausea, vomiting, constipation, and gingival hyperplasia (overgrowth of gum tissue). These side effects are generally dose-dependent and may be minimized by proper dose adjustment and adherence to the prescribed regimen.
More severe side effects can occur, particularly with long-term use. These include osteomalacia (softening of the bones), folate deficiency leading to megaloblastic anemia, and peripheral neuropathy. Chronic use of Phenytoin can also lead to cosmetic issues such as hirsutism (excessive hair growth) and acne.
Phenytoin has several contraindications. It should not be used in individuals with a known hypersensitivity to the drug or its components. Patients with a history of hepatotoxicity related to Phenytoin, or those with specific cardiac conditions like bradycardia or heart block, should avoid its use unless absolutely necessary and under close supervision.
One of the more serious risks associated with Phenytoin is the potential for Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), rare but life-threatening skin reactions. These risks are higher in individuals with certain genetic profiles, particularly those of Asian descent carrying the HLA-B*1502 allele. Genetic screening can help mitigate this risk.
Another important consideration is the drug’s potential impact on mental health, as it can cause mood changes, agitation, and, in rare cases, suicidal ideation.
What Other Drugs Will Affect Phenytoin
Phenytoin is known for its potential to interact with numerous other medications, which can either increase its toxicity or reduce its efficacy. It is metabolized by the cytochrome P450 enzyme system, specifically CYP2C9 and CYP2C19, making it susceptible to interactions with drugs that induce or inhibit these enzymes.
Enzyme inducers such as carbamazepine, phenobarbital, and rifampin can decrease Phenytoin levels, potentially leading to subtherapeutic effects and increased seizure risk. Conversely, enzyme inhibitors like valproic acid, cimetidine, and fluoxetine can increase Phenytoin levels, raising the risk of toxicity.
Other anticonvulsants can also interact with Phenytoin. For instance, valproic acid not only inhibits Phenytoin metabolism but also displaces it from plasma proteins, further increasing free Phenytoin levels.
Warfarin, a commonly used anticoagulant, is another drug that heavily interacts with Phenytoin. Both drugs can affect each other's metabolism, leading to either increased bleeding risk or reduced anticoagulant effect, necessitating close monitoring of coagulation parameters.
Oral contraceptives can be less effective when taken with Phenytoin due to its enzyme-inducing properties, which can increase the metabolism of estrogen and progesterone. This interaction necessitates the use of alternative or additional contraceptive methods.
Alcohol consumption can also influence Phenytoin levels. Acute alcohol intake can inhibit its metabolism, while chronic alcohol use can induce enzyme activity, leading to variable effects.
Patients should always inform their healthcare providers about all medications they are taking, including over-the-counter drugs and supplements, to carefully manage and adjust doses and avoid potential interactions.
In summary, while Phenytoin remains a vital tool in the management of epilepsy and other neurological conditions, its use requires careful monitoring and consideration of potential side effects and drug interactions. Proper patient education and regular follow-ups are essential to optimize therapeutic outcomes and minimize risks.
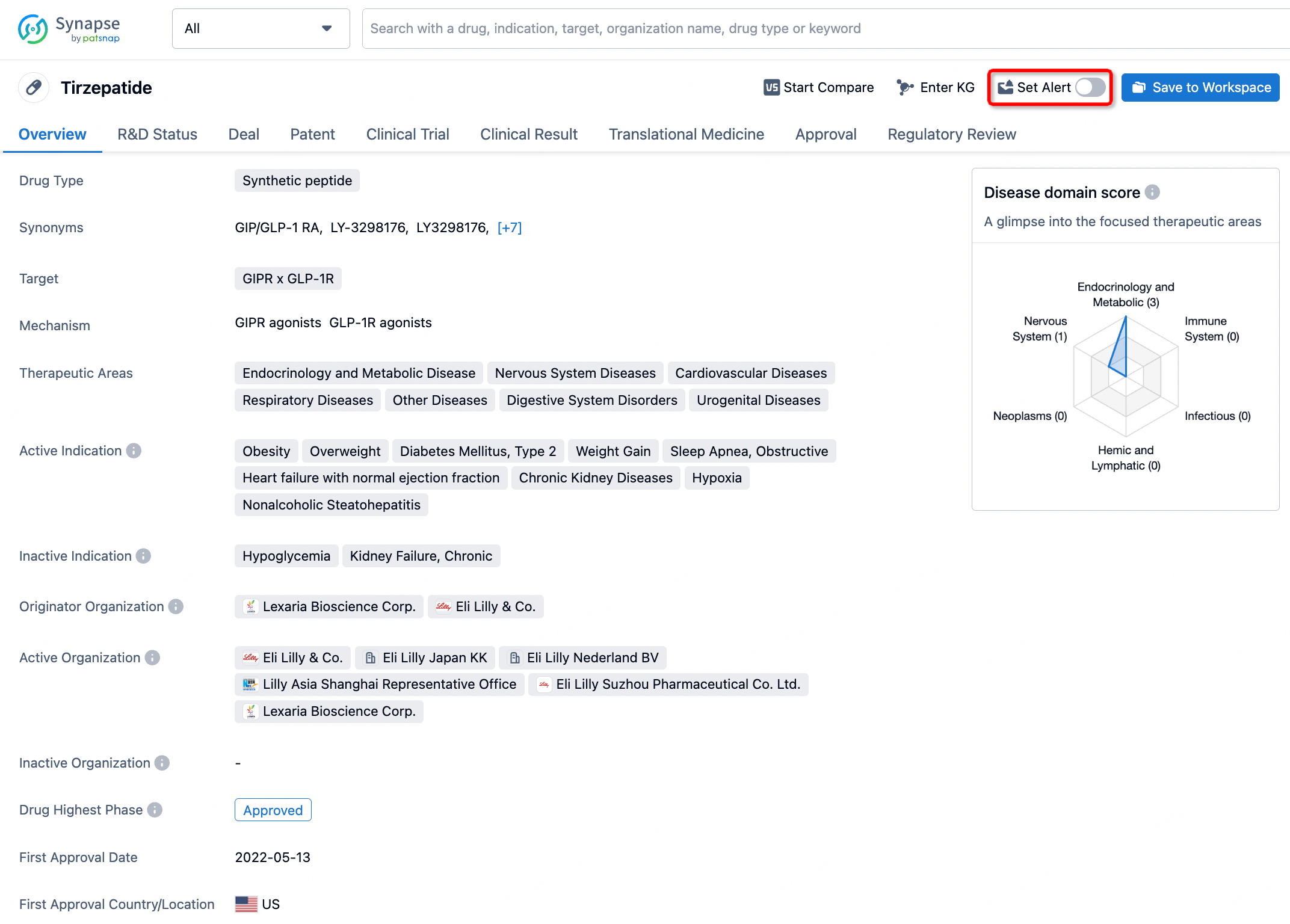
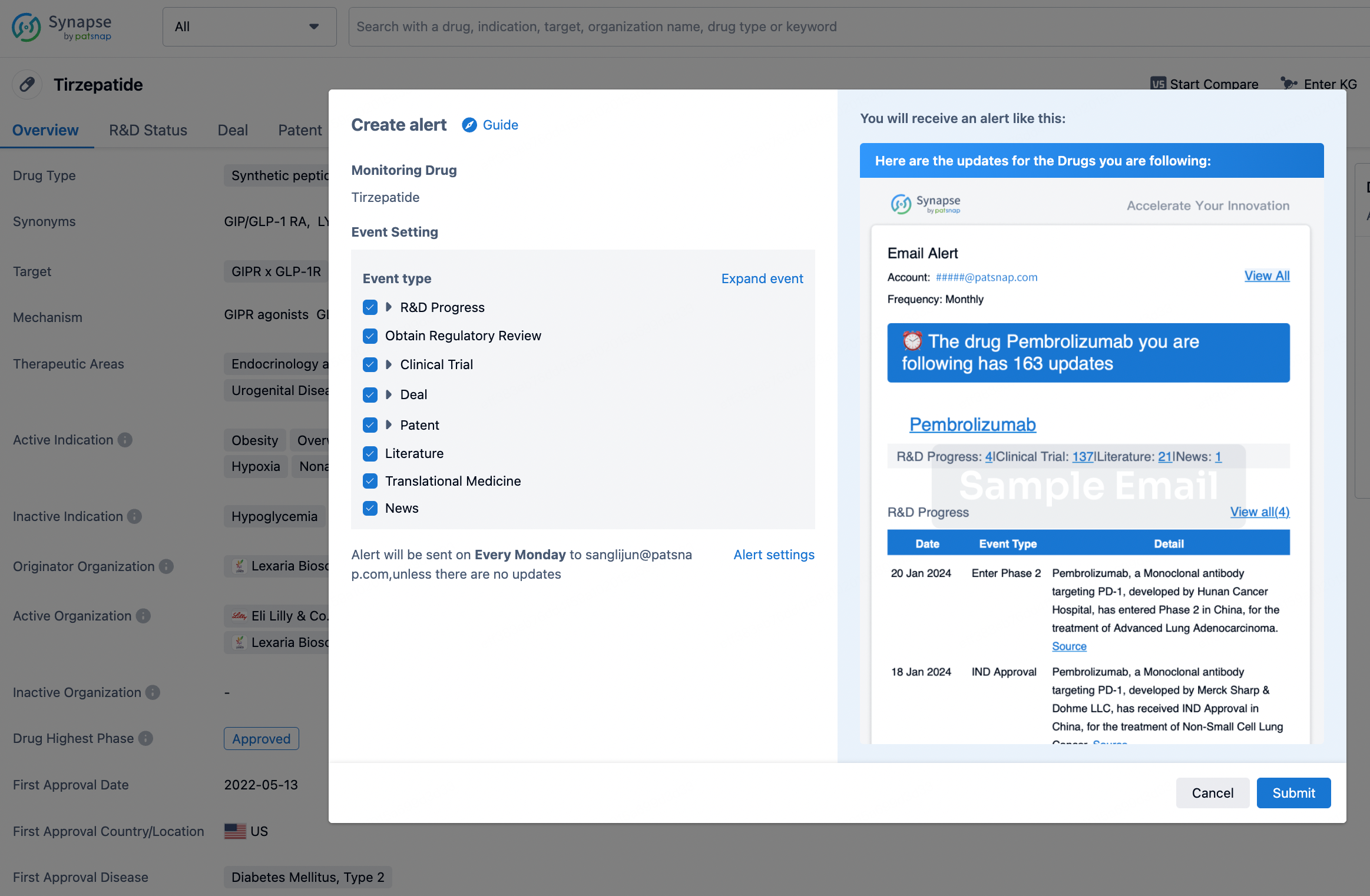
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.